What type of saliva is characterized as thick and mucus-rich?
Click to see answer
Mucous saliva (less in volume)
Click to see question
What type of saliva is characterized as thick and mucus-rich?
Mucous saliva (less in volume)
What is the composition of the lamina propria in the tunica mucosa?
Loose connective tissue (LCT).
What do you call the invagination in the tunica mucosa of the small intestine
Crypt of Lieberkuhn
What are the types of cells in the tunica mucosa
Goblet cells
enteroendocrine cells
lamina propria (loose connective tissue)
lamina muscularis mucosae
What are plica circulares?
Large mucosal folds that add to the intestinal surface area.
= the tunica mucosa are thrown into folds
more folds = increases the surface area for the contact of food material
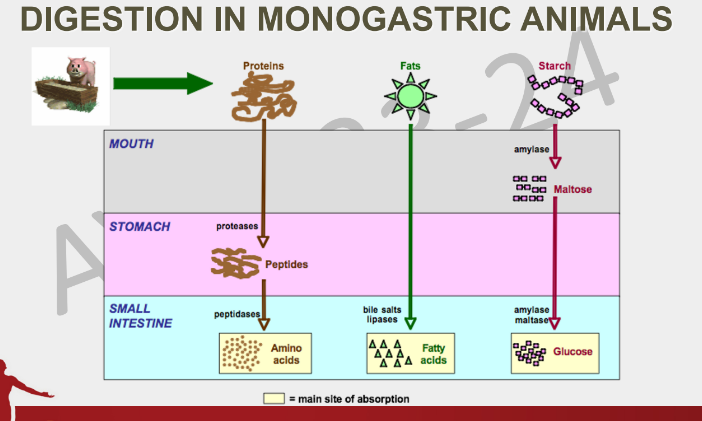
Where can you find the enterokinase of the small intestinal epithelial cell
In the brush border
What is the role of the enterokinase in the brush border of the small intestines
They activate Trypsinogen into trypsin which is the activator for chymotrypsinogen which will then be activated into chymotrypsin
What are the intestinal digestive enzymes
phospholipase A2
Nuclease
Nucleotidase
Nucleosidase
What are the carbohydrases in the intestines
maltase
lactase
sucrase
α-limit dextrinase
What are the small intestinal hormones secreted by the enteroendocrine cells particularly in the duodenum and jejunum?
Secretin
Cholecystokinin or Pancreozymin
Gastric Inhibitory Peptide (GIP) or Enterogastrone or Glucose-dependent Insulinotrophic Peptide
Vasoactive Intestinal Peptide (VIP)
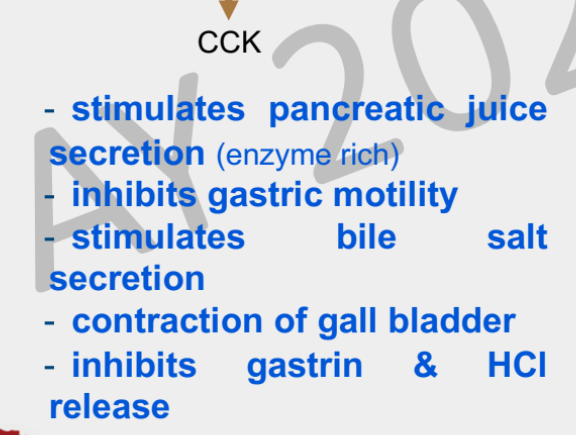
What is the role of CCK
Which is secreted first in the duodenum, CCK or secretin?
Both secretin and CCK are secreted simultaneously
What is the role of Secretin
What is the function of Gastric Inhibitory Peptide (GIP)?
a. inhibits gastric juice secretion
b. enhances insulin release
c. reduces contraction of gastric smooth muscles or gastric motility (to regulate the amount of chyme that enters the stomach)
What is the function of the thickening of the outer T. muscularis in the large intestine?
The taenia coli forms haustrations or sacculations, important for mixing and fermentation
What animals are the taenia coli prominent in?
Pigs and large animals
What do you call the thickening of the the outer tunica muscularis in the large intestine
Taenia coli
What is the importance of the taenia coli?
The taenia coli in the large intestines is characterized by the thickening of the outer tunica muscularis. When they contract, it forms haustrations or sacculations which are important for mixing and fermentation of food materials
What are the functions of the large intestine?
1.Site of absorption of water
2.Site of absorption of electrolytes
3.Site of microbial fermentation in non-ruminant herbivores (specially horses)
4.Storage of fecal matter until expulsion
5.Site of microbial fermentation in non-ruminant herbivores
6.Storage of fecal matter until expulsion
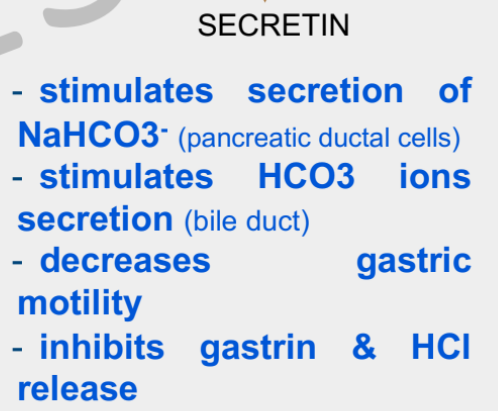
Describe the digestion process in monogastric animals
If we divide the alimentary canal, for proteins, the initial digestion of proteins takes place in the stomach because of the secretion of proteases such as pepsin which can digest our polypeptides into shorter peptides. These peptides will then go to the small intestine which will then be further digested into amino acids where these will be absorbed in the small intestine
Where and how are starch initially digested for hindgut fermenters?
For starch, there are 2 processes
Horses secrete salivary amylase which allow starch to be converted into maltose which will then be transported into SI. Here they will be acted upon by the pancreatic amylase and maltase that will digest it into glucose molecules
Horses are hindgut fermenters so they require carbohydrates to be fermented and acted upon by microbes such as bacteria. These microbial bacteria in the cecum would be converted into Volatile Fatty Acids = butyric acid, acetic acid, and propionic acid
Where and how are proteins initially digested for monogastric animals?
In the stomach, where proteases such as pepsin are able to digest these proteins from polypeptides to shorter peptides. These peptides then go into the small intestine to be further digested by peptidases into amino acids where they are absorbed in the small intestine
Where and how are fats initially digested for monogastric animals?
For monogastric animals = no initial digestion in the mouth
In the stomach, there is curdling particularly for the carnivores
Initial digestion takes place in the small intestine where bile salts allow the emulsification of fats while lipases are for the digestion of the fats into fatty acids and monoglycerols
Where and how are carbohydrates initially digested for monogastric animals?
Carbohydrates contain starch and they are initially digested into maltose through the action of salivary amylase within the oral cavity. Some of the starch and maltose will be transported into the small intestine where they can be further digested into monosacharide glucose by pancreatic amylase and maltase. The site of absorption for simple sugars are in the small intestine
Where and how are proteins initially digested for hindgut fermenters?
Proteins are initially digested in the stomach due to the production of pepsin where polypeptides are digested into shorter peptides. Most of the protein digestion takes place in the small intestine due to the action of intestinal peptidases and pancreatic peptidases. The product, amino acids, will then be absorbed in the small intestine
Where and how are fats initially digested for hindgut fermenters?
Fats are digested in the SI through the action of bile salts for emulsification and lipases for digestion. Its products, fatty acids and monoglycerols are absorbed in the the SI
Where and how are cellulose and hemicellulose initially digested for hindgut fermenters?
Horses eat roughages and the carbohydrates found here are cellulose and hemicellulose. There is no digestion taking place in the mouth, stomach and small intestine because animals do not have cellulase. Therefore, they are dependent on the microbial fermentation of the hindgut microbes to digest cellulose and hemicellulose to digest them into VFAs
Where are carbohydrates (CHO) digested in the digestive system?
NOT in the small intestine (SI), instead in the Large intestine
Where is the pancreas located?
In the duodenal loop
What are two main components of the pancreas?
Pancreatic Islet or Islet of Langerhans
Pancreatic acini (composed of the acinar cells, centroacinar cells, intralocular duct, and basket cells)
What is the role of the acinar cells in the pancreas?
These acinar cells are the ones producing the enzymes that are part of the pancreatic juice being released in the duodenum
What do you call the opening sphincter in the pancreatic duct leading to the duodenum?
Sphincter of Oddi
What is the role of the Sphincter of Oddi in the pancreas?
This sphincter opens in order to empty the pancreatic juice into the duodenum so that the enzymes can act on the components of the food ingested and at the same time, the sodium bicarbonate produced by the pancreatic ductile cells can act as a buffer in order to neutralize the acidity of the chyme
What are the 4 types of cells of the pancreatic islet
alpha cells
beta cells
delta cells
gamma cells
What is the role of the pancreatic juice rich in sodium bicarbonate?
It neutralizes the acidic pH of the chyme
What type of bonds does trypsin cleave?
Cleaves peptide bonds adjacent to Arg or Lys
What is the product of Carboxy-peptidase A activity?
Amino acids
What are the substrates for Trypsin, Chymotrypsin, and Carboxypeptidase A?
proteins
What is the product of Elastase activity?
short peptides
What is the product of Colipase activity?
It makes an anchor for lipase allowing it to bind to the bile salt-triglyceride-water interface
What is the substrate of Carboxy-peptidase B and Elastase?
proteins
What is the substrate of Colipase?
Fat droplets
What is the activator for Lipase (prolipase) activity?
Trypsin
What is the activator of pancreatic amylase activity?
Chlorine
What is the normal arrangement of hepatocytes
arranged radially, form cord-like arrangement
Explain the process of production for HCO3 ions by pancreatic ductular cells
The source of bicarbonate is from the CO2 from the blood vessels supplying the pancreas. As it enters the pancreatic ductular cells, water enters as well, and they mix to form carbonic acid. Carbonic acid (H2CO3) then dissociates into H ions and HCO3 ions. The bicarbonate and Na ions in the pancreatic ductular cells will be transported into the pancreatic duct lumen, and in this lumen, they will undergo coupling or binding to form sodium bicarbonate
What is another term for liver cells
hepatocytes
What do you call the spaces lined with epithelial cells that separates the hepatocytes
sinusoids
What do you call the phagocytic cells found in sinusoids in the liver?
Von Kuppfer cells
In the liver, what structure is formed with three lobules and why is it called this way
Portal triad
= called this way because it contains the:
hepatic/portal vein
hepatic artery
interlobular bile duct
= two of which are blood vessels
What is the functional unit of the liver that describes the organization of liver cells around the blood supply and where is it formed?
hepatic acinus
= formed between 2 hepatic lobules
What is the role of Zone 2 in the hepatic acinus?
= intermediately oxygenated
What is the significance of Zone 1 in the hepatic acinus?
It is the area closest to the portal triad and is involved in the uptake of nutrients and oxygen.
= where the hepatic artery and hepatic vein are located
= best oxygenated zone
= disadvantage = first to absorb blood-borne toxins from the portal blood making them the most vlunerable
Why is the liver a highly vascularized gland?
The products of digestion are delivered to the liver for metabolism therefore, it needs to be vascularized
What happens when there is an abnormality in the lymph production?
This causes an increase in pressure in the space of Disse in the liver. This will lead to an increased production in lymph which can lead to Ascites or the abnormal accumulation of fluids in the abdominal region of the animal
How is bilirubin excreted by the liver to eliminate the products of dying or damaged RBCs?
Blood contains hemoglobin, and this is where iron is attached. When this dissociates, it separates the heme, globin, and iron components. The heme component which contains bilirubin is toxic, and it goes out of the dead or damaged RBC and it goes to the blood plasma then it binds to albumin. The albumin then carries bilirubin through the blood and when it reaches the liver, it cleaves from the albumin and that free bilirubin undergoes conjugation with the glucuronic acid. This conjugated bilirubin will now be released into the bile and it will enter the bile canaliculi or the duct system and it will then be released into the small intestine. There, it will be acted upon by the small intestine forming the Urobilinogen and the stercobilinogen. The urobilinogen is responsible for the pale yellow color of the urine and this is the way it is excreted out of the body of the animal. The stercobilinogen would be excreted as feces and it is responsible for imparting the light brown color of feces
What minerals are stored in the liver?
Iron.
What happens to rennin activity as a person ages?
Rennin activity decreases with age.
Do ruminants have salivary amylase?
No.
Where does the absorption of Vitamin B12 occur?
In the ileum.
What is the primary function of the distal stomach?
Mixing, grinding, and sieving of food.
What does pancreatic esterase act on?
Cholesterol esters.
What stimulates the release of Cholecystokinin (CCK)?
The presence of peptides, amino acids, and fats in chyme in the duodenum.
What product does Enteropeptidase produce?
Trypsin.
Which water-soluble vitamin is stored in the liver?
Vitamin B12.
What are gall bladder stones commonly known as?
Choleliths.
What is one method used for the diagnosis of cholelithiasis?
Endoscopy - Choledoscopy.
How does blood flow through the hepatic acinus?
Blood flows from the portal triad through the sinusoids to the central vein.
What is one of the primary functions of the liver related to fat metabolism?
Oxidation of fats (triglycerides).
What does Intrinsic Factor bind to?
Vitamin B12.
What do Brunner's glands secrete?
Mucus.
What are proenzymes?
Inactive enzyme precursors that are activated in the digestive system.
How are bile salts reabsorbed in the distal ileum?
By active transport through enterocytes.
What type of saliva is characterized as thin and fluid-like?
Serous saliva (more in volume)
What are the main cations found in pancreatic juice?
Sodium (Na), Potassium (K), Calcium (Ca), Magnesium (Mg).
What structure forms the brush border of the small intestine?
Glycocalyx, along with microvilli.
What is the role of gastric juice in the formation of chyme?
It aids in the digestion of food.
What happens to pepsin at pH 5.0?
Pepsin is reversibly inactivated.
What do immunoglobulins (Ig) in mucus do?
Bind organisms or pathogens.
What enzyme acts on fats after emulsification?
Lipase.
What are the three main types of Volatile Fatty Acids (VFA)?
Acetic, propionic, and butyric acids.
Where does the absorption of electrolytes primarily occur?
In the large intestine.
What do mucus neck cells in the pylorus of the stomach secrete?
Mucus.
What are the main parts of the Large Intestine?
Cecum, Colon, Rectum, Anus.
What is the esophagus?
A muscular tube that connects the oropharynx to the stomach.
Contracts in order to transport food from the oropharynx into the stomach. This is possible because it is composed of skeletal muscles and for some, the caudal part is formed by smooth muscles
What does the soft palate separate?
The mouth from the nasopharynx.
What are the two layers of the tunica muscularis?
Inner circular arrangement of the smooth muscles and outer longitudinal arrangement of the 2nd layer of smooth muscles
What types of fats does the liver synthesize?
Cholesterol and phospholipids.
What is the primary function of the liver?
To process nutrients from the digestive system.
How does the liver contribute to glycogen storage?
It promotes glycogenesis in skeletal muscles and the liver.
What does a sweet taste usually indicate in animals?
Energy-rich nutrients.
Is salivary amylase present in dogs?
Yes.
What is the primary function of canines?
Cutting or shearing.
What are the distinct features of the tunica mucosa in the wall of the small intestine
Simple columnar absorptive epithelium with many Goblet cells.
What substance can cause liver cirrhosis?
Alcohol.
What is the primary function of premolars?
Chewing and grinding.
What are Goblet cells responsible for in the small intestine?
These pinkish-staining goblet-shaped cells secrete mucin that mixes with water to form mucous that coats the wall of the small intestine
What is cholelithiasis commonly known as?
Gall bladder stones.
What are the main anatomic structures involved in digestion?
Mouth, esophagus, stomach, small intestine, large intestine, and accessory glands.
How can abdominal pain from cholelithiasis vary?
It can range from mild to excruciating.
What is a key characteristic of avian digestion?
Birds have a crop for storage and a gizzard for grinding food.
Which animals are known to have a gall bladder?
Domestic animals such as horse, deer, elk, moose, giraffe, camel, elephant, and pigeon.
What is the function of microvilli in the small intestine?
To increase surface area for absorption.
How are bile salts reabsorbed in the cranial small intestine?
By diffusion through enterocytes.
Which cells are responsible for the production of HCO3 ions in the pancreas?
Pancreatic ductular cells.
What is the primary function of incisors?
Cutting or shearing.
What condition involving the gallbladder can lead to gallstones?
Inflammation of the gallbladder or bile duct epithelium.
Which structures are involved in the passage of food and air?
Oropharynx and larynx.
What are the intestinal enzymes secreted by enterocytes?
Peptidases or proteases (protein-digesting enzymes)
sucrase, maltase, isomaltase, lactase (carbohydrate-digesting enzymes)
intestinal lipase, and phospholipase (lipases that digest fats)
What is one function of the liver related to detoxification?
It serves as a detoxification gland.
What does the liver promote the synthesis of in relation to fats?
Lipoproteins.
What can cause incomplete emptying of the gallbladder?
Stasis of the gallbladder or bile duct.
What role does the kidney play in excretion?
It filters blood to remove waste products, including urobilinogen.
What is jaundice also known as?
Icterus.
What is a characteristic of bile in the gall bladder?
It has a high concentration of organic components.
Which disease states are associated with excess cholesterol leading to gallstones?
Obesity, acute high calorie intake, high fat diet, diabetes mellitus, hypercholesteronemia.
What does saliva contain that is similar to blood plasma?
Electrolytes.
What causes the formation of gall bladder stones?
Precipitation of cholesterol in the gall bladder and/or ducts.
Are plica circulares present in all animal species?
No, they are not present in all animal species.
What imaging technique is used to diagnose cholelithiasis?
Ultrasound.
What is one cause of gallstones related to bile composition?
Excess absorption of H2O in bile.
What is a primary function of lips in sheep, goats, and horses?
They serve as a prehensile organ, being soft and flexible.
How does mucus contribute to the small intestine's function?
Provides lubrication.
What is the primary function of the pancreas?
To produce digestive enzymes and hormones, including insulin.
What causes Zollinger-Ellison syndrome in dogs?
Gastrinoma, which are gastrin-secreting tumors
What are the four main components of the tunica submucosa?
connective tissues
nerves
blood vessels - supplies the GI tract
duodenal or Brunners glands
What are the lips classified as in relation to the mouth?
They are an associated structure of the mouth.
What are sinusoids in the liver?
Specialized blood vessels where blood enters.
Which macronutrient is likely to speed up gastric emptying?
Carbohydrates.
What is released from the liver to the duodenum?
Bile.
What substance does the liver produce that aids in digestion?
Bile.
What is the relationship between swallowing and respiration?
Swallowing temporarily interrupts normal respiration.
What is the purpose of proenzymes in the pancreas?
To aid in digestion once activated.
What is the role of emulsification of fats in digestion?
It increases the surface area of fat for lipase action.
What do mucus neck cells secrete?
Mucus.
What is the function of somatostatin secreted by delta cells?
It regulates the endocrine system and inhibits hormone secretion.
What is the substrate for maltase?
Maltose.
Name the specific proenzymes secreted by the pancreas?
= enteropeptidase or enterokinase
How does bile assist pancreatic lipase?
By increasing the surface area of fat for lipase action.
What can cause liver damage?
Toxins.
During which academic year is the study of gall bladder stones being referenced?
AY 2023 - 24.
What is the surgical procedure for treating cholelithiasis?
Cholecystectomy.
What action does rennet perform in cheese making?
It has the same action as rennin.
What is another product of microbial fermentation besides Volatile Fatty Acids?
Lactic acid.
What is renin used for?
Cheese making.
What is microbial fermentation?
The process of enzymatic decomposition and utilization of food by bacteria.
What percentage of blood in the liver is venous?
75%.
Which animal has the largest large intestine and what is its cecum shaped like?
Horse = comma-shaped cecum
What percentage of blood in the liver is arterial?
25%.
What is the primary function of the esophagus?
To propel food to the stomach.
What process helps convert large solid particles into smaller particles in the stomach?
Peristalsis and the opening of the pyloric sphincter.
What do you call the ganglion found in the middle of the inner and outer layer of the tunica muscularis?
myenteric ganglion plexus
What are the components of the colon in cows?
Ascending colon (spiral colon), very short transverse colon, descending colon.
How does gastrin affect gastric mucosa?
Promotes growth of gastric mucosa.
= Cells present in the organs have a lifespan. This means that the old and dying cells need to be replaced by new cells, including those in the gastric mucosa. This is the role of gastrin
Why does the deficiency in intrinsic factor and vitamin B12 lead to pernicious anemia
Vitamin B12 is important when it comes to the maturation of red blood cells
= This is why if there is a deficiency in intrinsic factor production, this will also lead to pernicious anemia which is characterized by the presence of immature red blood cells
What is the reason for microbial fermentation occurring in the large intestine?
Due to the presence of bacteria in the LI.
What are the components of the colon in pigs?
Ascending colon (spiral colon), transverse colon, descending colon.
How do proteins affect gastric motility?
Proteins can influence the rate of gastric emptying, but the effect is less pronounced than fats.
How frequently does Zollinger-Ellison syndrome occur in dogs?
It occurs with low frequency.
What role does the submucosa play in the alimentary canal?
It provides support and contains blood vessels, nerves, and glands.
Where is the upper esophageal sphincter located?
Closely associated with the larynx.
Where is bile stored?
In the gall bladder.
Besides mucous, what else do mucus neck cells produce?
HCO3- or bicarbonate ions
What is the pH level of saliva?
Slightly alkaline.
What are the products of maltase?
2 Glucose molecules
How are proenzymes activated?
They are converted into active enzymes in the digestive tract.
What is the significance of bile produced by the liver?
It helps emulsify fats for digestion.
What happens to the organic part of bile and the watery solution during secretion?
They mix together.
What is the substrate for the enzyme Pepsin?
Proteins & Polypeptides.
What type of substances promotes the synthesis of proteins in the liver?
Plasma proteins, including albumin, globulins, and clotting factors like fibrinogen.
What is the primary function of the alimentary tract?
A series of tubular glands for the transport of food.
What is the process that increases the surface area of fat for lipase?
Emulsification of fats.
What role do accessory digestive glands play?
They aid in the digestion process
What are the main zones of the hepatic acinus?
Zone 1 (periportal), Zone 2 (mid-zonal), and Zone 3 (centrilobular).
What forms the lateral border of the mouth?
The cheeks.
What is the primary physiological function of the stomach?
To break down food and mix it with digestive juices.
How do the cheeks aid in the chewing process?
They help position food between teeth for chewing.
What is the site of microbial fermentation in non-ruminant herbivores?
The large intestine.
What do mucus neck cells secrete?
Mucus.
What are microvilli?
Minute extensions at the apex of enterocytes that increase surface area for absorption.
= found in the villi
What is the oropharynx?
A common passageway for food and air.
Serves to transport food from the oral cavity to the esophagus
What gases are produced during microbial fermentation?
CO2 (most abundant), methane, H, and N.
What is metabolism in the context of digestion?
The process by which the body converts food into energy and nutrients.
How does the liver promote lipogenesis?
By converting excess carbohydrates and proteins into fats.
What disease is characterized by hypergastrinemia, which is excessive and unregulated secretion of gastrin?
Zollinger-Ellison syndrome in dogs
G cells become hyperactive leading to an increase in the production of gastrin
What role does Intrinsic Factor play in relation to Vitamin B12?
It protects Vitamin B12 from gastric and intestinal digestion.
What is gastrin, a linear peptide, synthesized as?
Preprogastrin
Gastrin is arising from a longer peptide known as preprogastrin which will eventually be cleaved into progastrin
Which vitamins are synthesized during microbial fermentation?
Vitamin K and B.
What are villi?
Finger-like projections that cover the small intestine mucous membrane.
= important in the absorptive capacity of the SI
= You can distinguish the duodenum, jejunum, and ileum based on the shape and depth of the invaginations of the villi
What hormone do G cells secrete?
Gastrin.
What are the minor salivary glands located on the tongue called?
Lingual glands.
What is one of the primary functions of gastrin?
Stimulates gastric acid secretion.
What is the optimal pH range for pepsin activity?
1.5 to 3.0 (very acidic)
What is the role of HCO3 ions produced by pancreatic ductular cells?
To neutralize stomach acid in the small intestine.
How does normal respiration occur?
Through the inhalation and exhalation of air.
What is the first part of bile secretion?
The organic part of bile.
What does pancreatic juice contain to neutralize the acidic pH of chyme?
Sodium bicarbonate (NaHCO3).
What is the length of the small intestine in cows?
151 feet.
What causes a gallbladder mucocele?
It can be caused by obstruction of the cystic duct or chronic inflammation.
Where are proenzymes secreted?
In the pancreas.
What is one function of teeth related to food preparation?
Cut and grind food.
What is a common symptom of cholelithiasis?
Minor indigestion.
What are the functions of the small intestine?
1. site of enzymatic digestion
2. site of absorption of digested food
3. site of absorption of vitamins
4. site of absorption of fluids
What are the minor salivary glands located in the lips called?
Labial glands.
What ions are produced by pancreatic ductular cells?
HCO3 (bicarbonate) ions.
What are the excretory products of hemoglobin (Hb)?
Bilirubin and urobilinogen.
What components make up chyme?
Food, water, and gastric juice.
How do the lips function in cattle and pigs?
They close the mouth and are stiff and immobile.
What are the two types of pancreatic secretions?
Pancreatic juice rich in enzymes
Pancreatic juice rich in NaHCO3 (sodium bicarbonate)
How does the gall bladder concentrate bile?
By reabsorbing water and electrolytes, up to 5 times.
What is the predominant circulating form of gastrin?
Gastrin-34 (big gastrin).
What hormones are produced by the pancreas?
Insulin and glucagon.
What percentage of bile salts is reabsorbed by the small intestine into the portal circulation?
95%.
What is the primary stimulus for gastrin secretion?
The presence of food (peptides, amino acids, calcium) in the stomach.
Gastrin is secreted by the G cells of the stomach when food enters the stomach
What is the Space of Disse?
The area where blood proteins and fluid enter from sinusoids.
What happens to pepsin at pH 7 to 8?
Pepsin is irreversibly inactivated.
What is mixed with food in the mouth to facilitate swallowing?
Saliva.
Is salivary amylase present in horses?
Yes.
What are the four main layers of the small intestine?
Mucosa, submucosa, muscularis, and serosa.
What is an incomplete digestive system?
A digestive system that has only one opening for both ingestion and excretion.
What is one of the primary functions of the tongue?
To maneuver food within the mouth for mastication
Which animals are considered hindgut fermenters?
Horses, rabbits, and some rodents.
What is the treatment for a gallbladder mucocele?
Treatment often involves surgical removal of the gallbladder (cholecystectomy).
What effect does Gastric Inhibitory Peptide (GIP) have on gastric motility?
It reduces contraction of gastric smooth muscles.
What is the outermost layer of the alimentary canal called?
The serosa.
What are bile salts in relation to total solutes?
They make up 1/2 of the total solutes.
What is the function of goblet cells in the small intestine?
To secrete mucus.
What are the products of Phospholipase A2?
Fatty acids and lysophospholipids.
What phospholipid is found in bile?
Lecithin.
What physiological process occurs in the proximal stomach to accommodate food?
Receptive relaxation of stomach to accommodate food with little if any pressure
= as the stomach is being filled up, the stomach controls the buildup of pressure to prevent bursting of stomach
What is one of the primary functions of the liver?
Serves as a storage site for vitamins and minerals.
What is the primary site of water absorption in the digestive system?
The large intestine.
What is the role of Zone 3 in the hepatic acinus?
It is the area farthest from the portal triad and is more susceptible to ischemia and toxic injury.
= poorly oxygenated
= near the central vein of the hepatic lobule
What is a characteristic of bile acids important for fat digestion?
They are lipid soluble.
What distinguishes simple stomach animals from ruminants?
Simple stomach animals have a single-chambered stomach, while ruminants have a multi-chambered stomach for fermentation.
What does cholecystectomy involve?
Surgical removal of the gall bladder.
What functional group is associated with bile acids?
Methyl group.
What structure forms the roof of the mouth?
Hard palate.
What function does the large intestine serve regarding fecal matter?
Storage of fecal matter until expulsion.
What are the functions of mucus in the small intestine?
1. lines & protects intestinal epithelium
2. for lubrication
3. binds bacteria
4. holds immunoglobulins (Ig) so that they can bind the organisms or pathogens
What factors influence the rate of gastric emptying?
The type of food ingested.
= Carbohydrates fastest, proteins next, fats slowest
What type of cells are G cells?
Enteroendocrine cells.
What is the primary function of the gall bladder?
Storage of bile.
What is one function of the liver related to glucose metabolism?
Promotes gluconeogenesis from amino acids and fats.
What do parietal or oxyntic cells produce?
Hydrochloric acid (HCl) and intrinsic factor.
What is the primary function of swallowing?
To move food from the mouth to the esophagus.
Which macronutrient is likely to slow gastric emptying?
Fats.
the stomach takes long to digest it that is why you wont feel hungry for a longer period of time
What are the components of the colon in horses
large ascending colon, transverse colon, small descending colon
What condition is caused by a deficiency in Intrinsic Factor?
Pernicious anemia.
What hormone is secreted by alpha cells in the pancreatic islets?
Glucagon.
What hormone do enteroendocrine cells (G cells) secrete?
Gastrin.
Where is bilirubin processed in the body?
In the liver.
In which part of the digestive system does microbial fermentation occur in domestic animals?
In the large intestine (LI).
What are the main types of digestive systems?
There are two main types: complete digestive systems and incomplete digestive systems.
Which minor salivary glands are found in the roof of the mouth?
Palatine glands.
Which cells are responsible for the secretion of intrinsic factor?
Parietal or oxyntic cells.
What hormone is produced by beta cells in the pancreatic islets?
Insulin.
What type of enzymes are peptidases?
Enzymes that break down peptides into amino acids.
What is the function of chymosin (rennin) in the digestive system?
It allows milk to stay longer in the stomach and aids in the digestion of milk proteins.
What is the enzymatic preparation used for cheese making?
Rennet.
Why is emulsification important in fat digestion?
It increases the surface area for lipase to act on.
What protective function do teeth serve?
They help in the mechanical digestion of food.
What is the semi-solid mixture produced by gastric digestion of food called?
Chyme.
What is the secretion of chief or zymogen cells?
Pepsinogen = the peptide activated to form pepsin
How does bile acid absorption contribute to gallstone formation?
Excess absorption of bile acids can lead to gallstones.
What does the oropharynx prevent?
The entry of food into the larynx and nasal cavity.
How is bilirubin formed?
From the breakdown of hemoglobin in red blood cells.
What is a gallbladder mucocele?
A condition characterized by the accumulation of mucus in the gallbladder.
What role does mucus play in relation to bacteria in the small intestine?
Binds bacteria.
What process helps in moving food through the esophagus?
Peristalsis.
What is the outermost layer of the digestive tract that comprises of a very thin layer of connective tissue?
Tunica serosa.
What is the pH level of pancreatic juice?
pH 8.0.
What is the length of the small intestine in sheep?
85 feet.
What are primary bile acids conjugated with to form secondary bile acids?
Taurine or Glycine.
What is the layer beneath the mucosa in the digestive tract?
Tunica submucosa.
Which domestic animal has the shortest and simplest large intestine?
Dog.
What is the primary function of molars?
Chewing and grinding.
What does Carboxypeptidase B cleave?
C-terminal amino acids that have basic side chains.
What is absent in the large intestine compared to other parts of the digestive system?
Villi.
What do intestinal lipase and phospholipase do?
They are enzymes that break down fats and phospholipids.
What type of stomach do monogastric animals have?
A single-chambered stomach.
What is the primary function of saliva?
To lubricate food.
What is one importance of the upper esophageal sphincter?
It routes food into the esophagus.
What is the inactive form of Trypsin?
Trypsinogen.
What is the primary function of bile acids and bile salts?
Their primary function is to aid in the digestion and absorption of fats in the small intestine.
What ions does Secretin stimulate the secretion of in the bile duct?
HCO3 ions.
What is one of the main components of bile besides bile salts?
Cholesterol.
What is the function of pepsin?
It cleaves or digests polypeptides into shorter peptides
Why is the secretion of mucus important?
It prevents damage to the gastric mucosa.
What process does the liver promote during malnutrition or starvation?
Glycogenolysis.
What is the typical taste associated with acids?
Sour.
What is a complete digestive system?
A digestive system with a separate mouth and anus, allowing for a one-way flow of food.
What is the primary function of salivary amylase?
To digest starch by hydrolyzing 1:4 α linkages in carbohydrates
What is the primary function of the hindgut in hindgut fermenters?
To ferment and digest fibrous plant material.
What percentage of total body lymph does the liver produce?
50%.
How does Gastric Inhibitory Peptide (GIP) affect insulin?
It enhances insulin release.
What does the mucus layer cover?
The gastric mucosa.
What is the normal color of feces in the presence of stercobilinogen?
Brown.
What type of cells are primarily found in the mucosa of the small intestine?
Columnar cells or enterocytes and goblet cells
What is the name of the secondary bile acid derived from Cholic Acid?
Deoxycholic acid.
Which cells produce gastric chymosin?
Gastric chief cells.
What enzyme in saliva is responsible for breaking down starch?
Salivary amylase or lingual ptyalin
What does Elastase cleave?
Bonds adjacent to aliphatic amino acids.
What are the Crypts of Lieberkühn?
Glands found in the mucosa of the large intestine.
What is the significance of the cecum in hindgut fermenters?
It is a major site for fermentation and absorption of nutrients.
How does the digestion process begin in monogastric animals?
With mechanical and enzymatic breakdown in the mouth.
Which part of the stomach contains mucus neck cells, chief cells, and parietal cells?
Fundus of the stomach.
What does lingual lipase digest fats into?
Free fatty acids (FFA) and diacylglycerol.
Where is the lower esophageal sphincter located?
Surrounds the esophagus just as it enters the stomach.
What is the activity of the lower esophageal sphincter during swallowing?
It is relaxed or open hence allowing food to pass going to the stomach
When they are not eating, it is closed and constricted
What does chyme in the duodenum stimulate?
Pancreatic juice secretion (enzyme-rich).
What size of food particles can pass through the pylorus into the small intestine?
Semi-liquid portions of food less than 2 mm in diameter.
What is the product of pancreatic esterase activity?
Cholesterol.
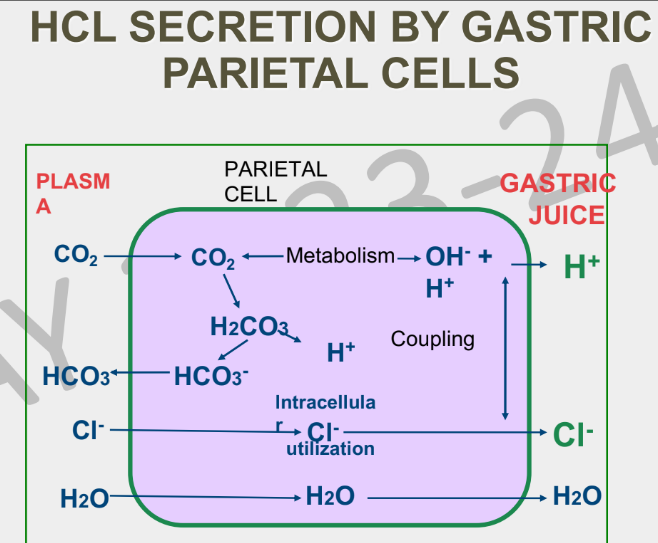
What is the relationship between H+ ions and HCl secretion?
H+ ions are a component of hydrochloric acid (HCl) secreted by parietal cells.
What role does chloride (Cl-) play in gastric juice composition?
It combines with H+ ions to form hydrochloric acid (HCl).
What does ribonuclease act on?
RNA.
What process occurs in the mouth that involves grinding and reducing the size of food particles?
Mastication or chewing.
Is salivary amylase present in pigs?
Yes.
What activates Procarboxypeptidase B?
Trypsin.
What triggers glycogenolysis in the liver?
States of malnutrition, hypoglycemia, or starvation.
What are the main anions present in pancreatic juice?
Bicarbonate (HCO3), Chloride (Cl), Sulfate (SO4), and Hydrogen Phosphate (HPO4).
What types of macromolecules does the pancreatic juice rich in enzymes help digest?
Carbohydrates (CHO), proteins, and fats.
What are the digestive enzymes produced by the pancreas?
Amylase, lipase, and proteases.
How many gastrin receptors are present in dog parietal cells?
44,000 gastrin receptors.
What is the muscularis layer responsible for?
It is responsible for the peristaltic movements that propel food through the canal.
How are enzymes secreted in pancreatic juice?
As proenzymes.
What is the importance of the bicarbonate ions secreted by the mucus neck cells
they are trapped in the mucous layer in the gastric mucosa and they neutralize the acids found in the gastric lumen in order to prevent damage to the gastric mucosa
What does Secretin stimulate in pancreatic ductal cells?
Secretion of NaHCO3.
What is a site for the conjugation of drugs?
The liver.
Which amino acids does the liver help synthesize?
Non-essential amino acids
= Skeletal muscles and liver are the two body structures that can synthesize non-essential amino acids therefore, they may not be supplied through the diet
What are the components of the distal stomach?
The last two-thirds of the body of the stomach and the pylorus.
What product does Aminopeptidase produce?
Short peptides.
What role do parietal cells play in digestion?
They produce hydrochloric acid (HCl).
What is Lithocholic acid classified as?
A secondary bile acid.
What is the role of taste buds in the tongue?
To provide the sense of taste.
How does the digestive process differ in hindgut fermenters compared to ruminants?
Hindgut fermenters digest food after it has passed through the stomach, while ruminants digest it in multiple stomach chambers.
What effect does Vasoactive Intestinal Peptide (VIP) have on gastric motility?
It reduces contraction of gastric smooth muscles.
What is the substrate for Dipeptidase?
Dipeptides.
What ions are exchanged in the process of HCl secretion by gastric parietal cells?
Bicarbonate (HCO3-) and chloride (Cl-).
What is the role of accessory glands in monogastric digestion?
They secrete enzymes and digestive juices to aid in digestion.
What does the lower esophageal sphincter prevent?
Gastric reflux of stomach contents.
What are the products of Nucleosidase?
Nucleic acids.
What is the function of the mucosa layer in the alimentary canal?
It is responsible for secretion, absorption, and protection.
What constitutes the second part of bile secretion?
A watery solution containing sodium (Na) and bicarbonate (HCO3) from ductal epithelial cells.
What are the potential symptoms of a gallbladder mucocele?
Symptoms may include abdominal pain, nausea, and vomiting.
What is the process called that involves the circulation of bile salts between the liver and the intestine?
Enterohepatic circulation.
Which gland is classified as serous based on its secretion type?
Parotid gland.
What color does urine typically appear due to urobilinogen?
Pale yellow.
What are the antimicrobial agents found in saliva?
IgA, lysozyme, lactoferrin, and thiocyanate ions.
What is the primary bile acid that can be conjugated to form Taurocholic acid?
Cholic Acid.
What role does the liver play in detoxification?
It filters toxins from the blood.
What is the term for the act of swallowing?
Deglutition.
What is the length of the small intestine in pigs?
60 feet.
What is the role of HCl in relation to pepsin?
HCl activates pepsinogen to pepsin.
What role do microbes play in hindgut fermentation?
They help break down cellulose and other complex carbohydrates.
What does the small intestine receive from the liver?
Bile via the common bile duct.
Which organisms typically have an incomplete digestive system?
Many cnidarians and flatworms.
What causes jaundice?
Accumulation of excessive amounts of free or conjugated bilirubin in the extracellular fluid (ECF).
What is the pathway of bile flow?
Bile flows to the common bile duct.
What role does cholesterol play in bile acid formation?
Cholesterol is the precursor for the synthesis of bile acids in the liver.
What protective function does the acidity of gastric secretion serve?
It poses a barrier to microbial invasion of the gastrointestinal tract.
What type of bonds does Chymotrypsin cleave?
Peptide bonds adjacent to aromatic amino acids.
What is the catalytic function of Pepsin?
Cleaves peptide bonds adjacent to aromatic amino acids into short peptides
What is the product of both Trypsin and Chymotrypsin activity?
Short peptides.
What is one importance of the lower esophageal sphincter?
It routes food into the stomach.
What is the substrate for Enteropeptidase?
Trypsinogen.
What is the enzyme that coagulates or curdles milk allowing it to turn from liquid to solid consistency?
Rennin or Chemosin or Chymosin.
What is the substrate for Nucleosidase?
Nucleosides.
What are the main functions of the liver?
Bile production, metabolism, detoxification, and storage of nutrients.
What are the two types of cells involved in pancreatic secretion and what do they secrete?
Pancreatic acinar cells = pancreatic juice rich in enzymes
pancreatic ductal cells = pancreatic juice rich in sodium bicarbonate
What are the minor salivary glands located near the zygomatic bone called?
Zygomatic glands.
Where are gastrin receptors located?
In parietal cells.
When gastrin binds to these gastrin receptors in the parietal cells, it stimulates the parietal cells to produce Hydrochloric acid
What is the primary site of protein metabolism and utilization in the body?
The liver.
What structures are involved in the swallowing process?
Mouth, pharynx, and esophagus.
What are the two main regions of the stomach?
Proximal stomach and distal stomach.
What is the inactive proenzyme that is converted to active chymosin?
prochymosin
What is the role of antimicrobial agents in saliva?
Protects oral mucosa and maintains oral hygiene.
How are bile salts formed?
Bile salts are formed by the conjugation of bile acids with amino acids, primarily glycine and taurine.
What type of cells are abundant in the large intestine?
Goblet cells and crypt of Lieberkuhn
= The large intestine as it goes distally, there is an increase in goblet cells since we need the mucous for the binding of the fecal material and it will also facilitate the transport and elimination of the fecal material
What are the visible signs of jaundice?
Yellowish discoloration of mucous membranes, skin, and sclera.
What type of enzyme is pepsin?
Endopeptidase.
Why is slow emptying of food from the stomach important?
For proper digestion and absorption.
What are the products of lactase?
Glucose and galactose.
What product does Pepsin produce?
Short peptides.
What is the substrate for sucrase?
Sucrose.
What is the significance of bile salts in the digestive process?
Bile salts emulsify fats, increasing their surface area for digestive enzymes to act upon.
What are the excretory products of hemoglobin found in bile?
Bilirubin and biliverdin.
What is the inactive form of Carboxy-peptidase A?
Procarboxy-peptidase A.
What is the product of α-limit dextrinase?
Glucose.
How does the liver contribute to metabolism?
By regulating blood sugar levels and storing glycogen.
Which compound is associated with vitamin B12?
Aldehydes.
Why is salty taste important for animals?
It allows modulating diet for electrolyte balance.
What is the length of the small intestine in horses?
73 feet.
What are bile acids?
Bile acids are steroid acids found predominantly in the bile of mammals, synthesized from cholesterol.
What type of cells are Hormone-secreting cells in the small intestine?
enteroendocrine cells
What do gamma cells in the pancreatic islets secrete?
Polypeptides.
What process does the liver promote for the removal of ammonia (NH3) from the body?
Conversion of NH3 to urea.
= this urea is from the catabolism of skeletal muscles that leads to the formation of ammonia. This ammonia is transported from the skeletal muscle cells to the liver and it is converted into urea, and eliminated through urine
Which organisms typically have a complete digestive system?
Most vertebrates and some invertebrates.
What ions are trapped in the mucous layer?
HCO3- ions.
What is the taste of amino acids called?
Umami.
What is the substrate for Phospholipase A2?
Lecithin.
What is the function of the lamina muscularis mucosae in the small intestine?
Contains smooth muscles.
What is the alternative name for Cholecystokinin?
Pancreozymin (PZ).
What does the small intestine receive from the pancreas?
Pancreatic juice via the hepatic duct.
What effect does bile have on the pH of intestinal chyme?
It produces an alkaline pH for optimal absorption.
What are the two key enzymes involved in the deamination and transamination of amino acids?
Alanine amino transferase (ALT) and aspartate amino transferase (AST).
What are the two layers of the T. muscularis in the large intestine?
Inner circular layer and outer longitudinal layer.
What can non-nitrogenous molecules be converted to in the liver?
Glucose or lipids.
What product does Dipeptidase produce?
2 amino acids.
What is the product of Carboxy-peptidase B activity?
Amino acids
What is the site of bile secretion?
The liver.
What are the products of deoxyribonuclease activity?
Nucleotides.
What is the function of sucrase, maltase, isomaltase, and lactase?
They are enzymes that break down sugars.
What is the primary focus of digestion in monogastric animals?
The breakdown of food in a single-chambered stomach.
How is a gallbladder mucocele diagnosed?
It is typically diagnosed through imaging studies like ultrasound or CT scan.
Which cells produce pepsinogen?
Gastric Chief Cells.
Which gland is classified as mucous based on its secretion type?
Mandibular gland.
What is Secretin?
A hormone involved in the digestive process.
Where is bile emptied into?
The duodenum.
What is the function of intestinal micelle formation?
It aids in the transport and absorption of digested fat products.
What is Cholecystokinin (CCK)?
A hormone that stimulates the digestion of fats and proteins.
What are the conjugated forms of Chenodeoxycholic acid?
Taurochenodeoxycholic or Glycochenodeoxycholic acids.
What is the primary function of parietal cells in the stomach?
Secretion of hydrochloric acid (HCl).
What vitamins are absorbed with the help of bile?
Fat-soluble vitamins.
What does the upper esophageal sphincter prevent?
Entry of air into the gastrointestinal tract.
What activates Procolipase?
Trypsin.
What does Aminopeptidase cleave from peptides?
N-terminal amino acid.
What role does the stomach play in monogastric digestion?
It further breaks down food using acids and enzymes.
Where are mucus neck cells located?
In the cardia of the stomach.
What is the function of the small intestine in monogastric animals?
Absorption of nutrients and further digestion.
What triggers the release of Secretin?
The presence of chyme in the duodenum.
What products does Gastric Lipase produce?
Fatty acids & Glycerol.
What does Carboxy-peptidase A cleave?
Carboxy terminal amino acids that have aromatic or aliphatic side chains.
What is the overall function of pancreatic digestive enzymes?
To cleave proteins into short peptides and amino acids.
Which animals are known to lack a gall bladder?
Animals without a gall bladder include certain species like some domestic animals.
What stimulates duodenal cells to secrete CCK and Secretin?
Chyme in the duodenum.
What variations exist in the cecum and colon among species?
Shape and size.
What does a bitter taste help animals sense?
Diverse natural toxins.
What are the components of the proximal stomach?
Cardia, fundus, and the first third of the body of the stomach.
How does the tongue assist in digestion?
By transporting food to the esophagus.
What is the substrate for lactase?
Lactose.
What activates Trypsinogen?
Entero-peptidase.
What is the role of carbon dioxide (CO2) in parietal cell metabolism?
It is converted into bicarbonate (HCO3-) and protons (H+).
What is the significance of glucagon?
It raises blood sugar levels when they are too low.
What is the substrate for Nuclease?
Nucleotides.
What waste product does bile help excrete?
Bilirubin.
What are the products of Nuclease?
Nucleic acids.
What is the substrate for α-limit dextrinase?
α-limit dextrin.
What is the primary solvent in bile?
Water.
What does CCK inhibit the release of?
Gastrin and HCl.
What substrate does pancreatic amylase act on?
Starch.
What is the product of pancreatic amylase activity?
Maltose.
What are the products of ribonuclease activity?
Nucleotides.
How does the pancreas contribute to digestion?
By secreting enzymes into the small intestine to aid in the breakdown of food.
What activates Proelastase?
Trypsin.
What is the substrate for Aminopeptidase?
Polypeptides.
What is the role of Vasoactive Intestinal Peptide (VIP)?
What is the function of HCO3- ions in the gastric lumen?
They neutralize acid.
What is the role of insulin?
To regulate blood sugar levels.
What is the proenzyme form of lipase?
Prolipase.
What is the primary function of the proximal stomach?
Storage and retention of ingested food.
What effect does Secretin have on gastric motility?
It decreases gastric motility.
How many amino acids does Secretin have?
27 amino acids.
What is formed when water (H2O) reacts with carbon dioxide (CO2) in parietal cells?
Carbonic acid (H2CO3).
What are the products of sucrase?
Glucose and fructose.
What is the role of Intrinsic factor in Vitamin B12 absorption?
It binds to Vitamin B12 to protect it from gastric and intestinal digestion.
What is the end product of the metabolic process in parietal cells?
Hydrochloric acid (HCl).
What are the products of Nucleotidase?
Nucleic acids.
What does Enteropeptidase cleave?
Peptide bonds adjacent to Arginine or Lysine.
What type of enzymes are Phospholipase A2, Nuclease, Nucleotidase, and Nucleosidase?
Intestinal digestive enzymes.
What does deoxyribonuclease act on?
DNA.
How does Vasoactive Intestinal Peptide (VIP) influence insulin?
It enhances insulin release.
What are the four layers of the large intestine?
T. mucosa, T. submucosa, T. muscularis, T. serosa.
What does lipase act on?
Triglycerides.
What does Secretin inhibit the release of?
Gastrin and HCl.
What are the products of lipase activity?
Fatty acids and monoglycerides.
What role do fatty acids play in bile?
They are one of the components of bile.
What does CCK stimulate in relation to the gall bladder?
Contraction of the gall bladder.
What is the significance of bicarbonate (HCO3-) in parietal cell function?
It helps maintain pH balance and is exchanged for chloride ions.
What type of enzymes are maltase, lactase, sucrase, and α-limit dextrinase?
Intestinal digestive enzymes (carbohydrases).
Which group of animals has less Gastric Lipase activity?
Herbivores.
What process allows the curdling of milk?
The conversion of casein to paracasein.
Which structures contain taste buds on the tongue?
Lingual papillae such as circumvallate and foliate.
How many amino acids does Cholecystokinin (CCK) have?
8 amino acids.
What is the substrate for Gastric Lipase?
Triglycerides.
What is the substrate for Nucleotidase?
Nucleotides.
What activates Procarboxy-peptidase A?
Trypsin.
Which electrolytes are found in bile?
Sodium (Na), Potassium (K), Chloride (Cl), Calcium (Ca), and Bicarbonate (HCO3).
In which type of animal is Rennin primarily found?
Only in young ruminants.
Which group of animals has more Gastric Lipase activity?
Carnivores.
What vitamins are stored in the liver that are fat-soluble?
Vitamins A, D, E, and K.
What are the differerent types of animals based on thier digestive systems?
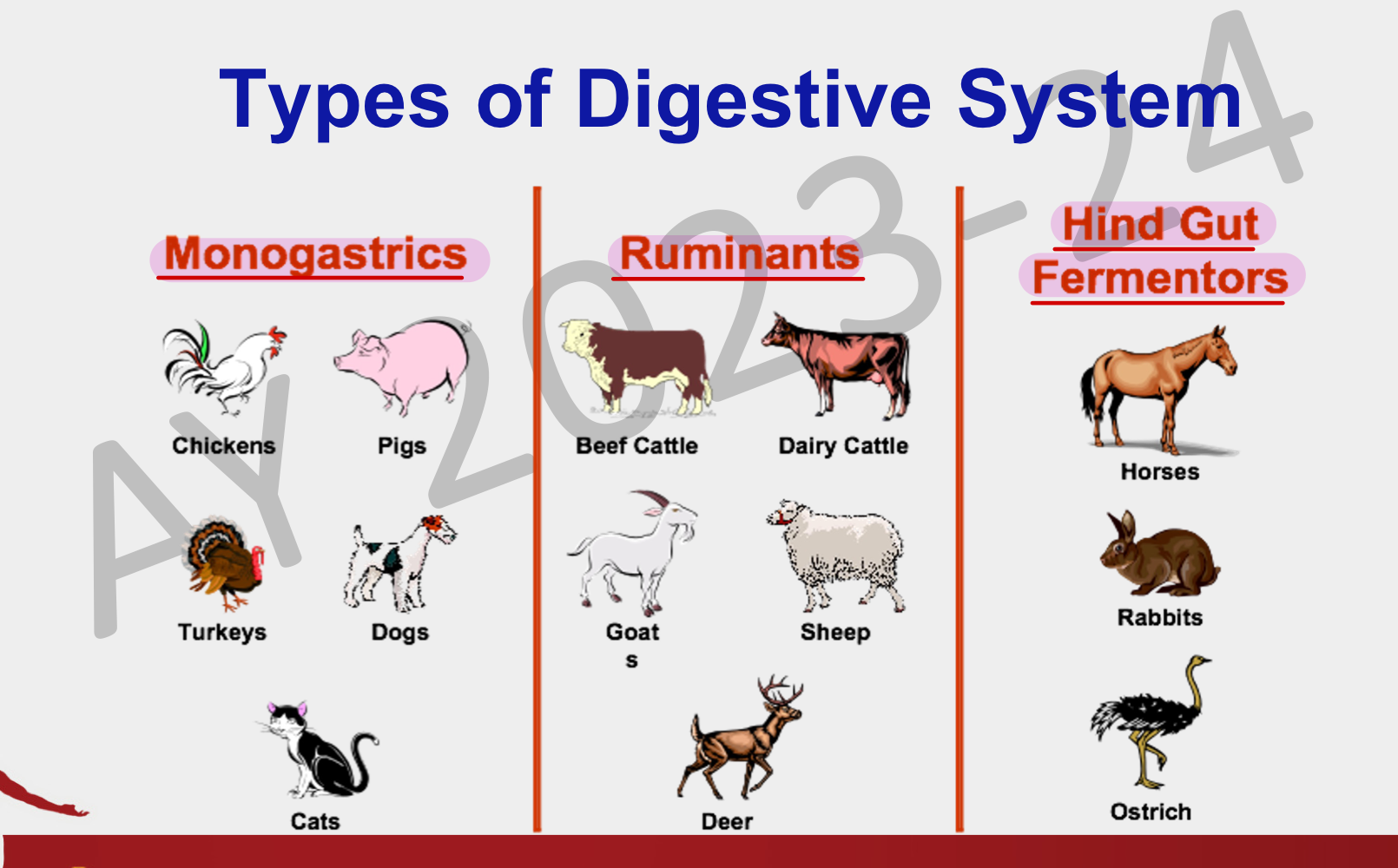
Differentiate monogastrics, ruminants, and hind gut fermenters
Here’s a breakdown of the three types of digestive systems: monogastrics, ruminants, and hindgut fermenters:
1. Monogastrics
- Definition: Monogastric animals have a single-chambered stomach.
- Digestive Process: Food is broken down primarily by stomach acids and enzymes. Digestion is relatively quick compared to other systems.
- Examples: Pigs, dogs, humans.
- Diet: These animals typically consume concentrated foods such as grains and meat, which are easier to digest in a single stomach.
2. Ruminants
- Definition: Ruminants have a complex, multi-chambered stomach, usually with four compartments: the rumen, reticulum, omasum, and abomasum.
- Digestive Process: They rely on microbial fermentation in the rumen to break down fibrous plant material like cellulose. After initial digestion, they regurgitate and re-chew food (cud), allowing for more complete nutrient extraction.
- Examples: Cattle, sheep, goats.
- Diet: These animals primarily consume fibrous plants such as grasses and hay, which are broken down slowly by microbial fermentation.
3. Hindgut Fermenters
- Definition: Hindgut fermenters have a single stomach, but their primary digestion of fibrous plant material occurs in the large intestine and cecum, rather than the stomach.
- Digestive Process: Food passes quickly through the stomach and small intestine, with microbial fermentation occurring in the large intestine and cecum to break down fibrous plant material.
- Examples: Horses, rabbits, guinea pigs.
- Diet: These animals primarily consume fibrous plants and vegetation, but digestion of cellulose occurs in the hindgut rather than in a fore-stomach like ruminants.
In summary, monogastrics digest food with a single stomach, ruminants ferment food in a multi-chambered stomach, and hindgut fermenters rely on microbial digestion in their large intestines or cecum.
What is the primary structure of the alimentary canal wall?
It consists of four main layers: tunica mucosa (innermost), tunica submucosa, tunica muscularis, and serosa (outermost).
What do you call the space in the alimentary canal wall
Lumen
What is the primary function of the mouth or oral cavity?
To receive food. Initial site of mastication
What are the 4 types of teeth
Incisors, Canines, Premolars, molars
frontal = incisors and canines
Back = premolars and molars
How do teeth contribute to digestion?
By increasing the surface area for chemical and microbial digestion of food.
= In Some species of animals, they have enzymes that can initially digest food in the oral cavity
What type of organ is the tongue considered in certain animals like cattle, buffalo, dogs and cats?
A prehensile organ.
What are the 5 types of tastes?
Sweet, sour, salty, bitter, umami
What are the 2 types of palate in the mouth
Hard palate and soft palate
What is a unique feature of ruminants related to the cheeks?
They have large papillae that aid in mastication and they play a large role in protecting the cheek mucosa from any rough feeds or roughage that are consumed by ruminants
What are the major salivary glands in dogs and cats?
Parotid (base of the ear), mandibular, zygomatic, sublingual
What are the minor salivary glands?
labial, buccal, lingual, palatine, zygomatic
Which minor salivary glands are found in the cheeks?
Buccal glands.
What is the dense 'sugar coating' of mucins important for?
It provides water-holding capacity and makes them resistant to proteolysis, which is important for mucosal barriers.
How is mucous formed?
When the mucin excreted by the salivary glands mixes with water
What is the importance of mucous?
Mucous is important as it coats the oral mucosa, protecting it from proteolysis
What are the serous secretory units in salivary glands?
Serous acinus which are responsible for the production of the serous type of saliva
Describe the appearance of mucous cells
Hazy appearance of the cytoplasm due to the presence of mucin
Which gland is classified as mixed based on its secretion type?
Sublingual gland.
What type of cells are found in the sublingual gland which are a combination of serous acinus and mucous cells
Serous demilune cells
What is the function of mucin in saliva?
Lubricates food, protects oral mucosa (by forming a mucous barrier), and controls the viscosity of saliva.
What is lingual lipase and when is it present?
Lingual lipase is an enzyme that digests milk fats to free fatty acids and diacylglycerol, and and is present in suckling calves (still feeding with milk)
What happens to lingual lipase when we shift the diet of the calf from milk to concentrates and roughages
The capacity of the salivary glands to produce lingual lipase disappears
What products are formed when salivary amylase digests starch?
Maltose, maltotriose, and α limit dextrins are formed through the hydrolysis of the 1:4 α linkages
What is the function of lingual lipase in calfs?
Initial break down of milk fats in the mouth.
What are the 7 functions of saliva
1. lubricates food
2. forms food boluses
3. facilitates swallowing
4. oral hygiene
5. solubilizes dry food
6. digestive function
7. evaporative cooling effect
What happens to the airway during swallowing?
The airway is closed off to prevent aspiration.
When swallowing food, the epiglottis closes off in order to prevent the entry of food in the trachea
During normal respiration, the epiglottis serves as a gate in order to block the entry of air into the esophagus, so when the animal inspires, the air is directed into the trachea
What are the two esophageal sphincters and what is their role?
The upper esophageal sphincters and the lower esophageal sphincter
= To regulate the transport of food
What is the activity of the upper esophageal sphincter during swallowing?
It is relaxed or open hence allowing food to pass through the esophagus
When they are not eating, it is closed and constricted
Differentiate the regions of the stomach of different types of animals
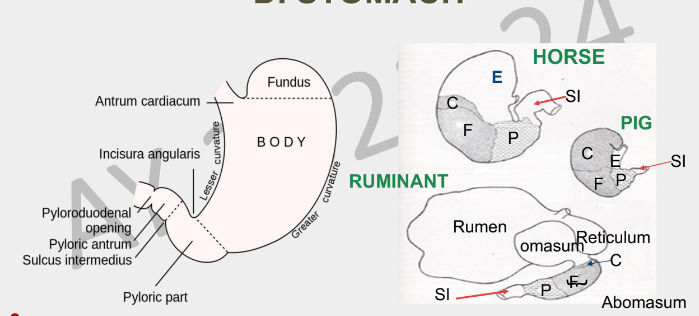
Left pic = monogastric animals
E= main body of the stomach
C= cardiac region
F= fundic region
P= pyloric region
SI = small intestine
What type of cells are found in the cardia of the stomach
Mucus neck cells.
What are the 4 types of cells found in the fundus of the stomach
Mucus neck cells
Chief or zymogen cells
Parietal or oxyntic cells
Gastrin-secreting or G cells
What are the 3 forms of gastrin and which among them is the longest?
Gastrin-34 (with 34 amino acids = longest)
Gastrin-17
Gastrin-14
What lesions are associated with Zollinger-Ellison syndrome?
Gastric and duodenal ulcerations.
Since gastrin promotes parietal cell secretion of hydrochloric acid, there would be an excessive production of hydrochloric acid which can result to ulcerations in the stomach
These gastric juices together together with food forms chime and it spills over to the duodenum, hence, its acidic condition would can lead to duodenal ulcerations
Describe the process by which the parietal cells produce HCl
When gastrin binds to the gastrin receptors in the parietal cells, this will stimulate the parietal cells to produce HCl (hydrochloric acid). The source of H ions comes from the dissociation of H2CO3 (carbonic acid) into H+ and HCO3 (bicarbonate). The bicarbonate ions are transported back to the blood plasma while the H ions are transported together with Cl to undergo coupling or binding in the parietal cells to form HCl in the lumen. HCl then binds with water in the gastic lumen to form the components of the gastric juices
What are the primary functions of the stomach?
1. storage of food
2. mixing of food with gastric juice (allowing it to interact with the secretions for its digestion)
3. digestive function
4. slow emptying of food from stomach to small intestine - for proper digestion and absorption
5. protective function - acidity of gastric secretion pose a barrier to microbial invasion of GIT
6. absorption of Vitamin B12 (ileum) - Intrinsic factor: binds to Vitamin B12 to protect it from gastric & intestinal digestion