What are the problems associated with complete decongestive surgery for lymphoedema?
Click to see answer
Click to see question
What are the problems associated with complete decongestive surgery for lymphoedema?
What pharmacological treatments are used for lymphoedema based on aetiology?
Aetiology | Treatment Options |
|---|---|
Filariasis | - Albendazole |
- Diethycarbamazine | |
Cellulitis | - Antibiotics |
** Diuretics are relatively contraindicated
What are the general complications of soft tissue injuries?
What is the normal anatomy of the nasolacrimal system?
What potential complication arises from injuries to the medial aspects of the eye?
Injuries to the medial aspects of the eye may result in permanent tearing if not repaired appropriately. It is important to consult OVS if damage is suspected.
What is the management for nasolacrimal system injuries?
Use silicon tubes to maintain patency of the drainage while the laceration heals.
What are the branches of the facial nerve and their associated muscles?
| Branch | Associated Muscles |
|---|---|
| Temporal Branch | Frontalis |
| Zygomatic Branch | Orbicularis oculi |
| Buccal Branch | Orbicularis oris, Buccinator, Zygomaticus |
| Marginal Branch | Mentalis |
| Cervical Branch | Platysma |
What is Pitanguy's Line and its significance?
Pitanguy's Line is located 0.5 cm below the tragus to 1.5 cm above the lateral eyebrow and is used for delineating the frontotemporal branch (temporal branch) of CN7.
What are the components of a Tripod (Tetrapod) fracture?
A Tripod (Tetrapod) fracture involves the following combining fractures:
What is a common type of fracture that involves the nasal area?
A Nasal bone fracture is a common type of fracture that is often detailed in ENT (Ear, Nose, and Throat) contexts.
What is the significance of understanding the components of a Tripod fracture in clinical practice?
Understanding the components of a Tripod fracture is crucial for:
What are the components of the Primary Survey in the ATLS Protocol?
The components of the Primary Survey in the ATLS Protocol are Airway, Breathing, and Circulation.
What are the three main causes of airway obstruction in facial trauma?
The three main causes of airway obstruction in facial trauma are:
What are the key findings in the physical examination of the upper face during a trauma assessment?
Key findings in the physical examination of the upper face include:
What signs might indicate an orbital injury during a physical examination?
Signs that might indicate an orbital injury include:
What is the gold standard investigation for facial fractures?
The gold standard investigation for facial fractures is a Plain CT Facial Bone plus Coronal Reconstruction.
What are the management steps for facial fractures?
The management steps for facial fractures include:
What are the associated injuries to look for in facial trauma?
Associated injuries to look for in facial trauma include:
What is the primary difference between a skin graft and a skin flap?
A skin graft is detached tissue without its own blood supply, requiring re-vascularization, while a skin flap is tissue that retains its own blood supply.
What factors should be considered when selecting a donor site for a skin graft?
Consider the following factors for donor site selection:
Additionally, avoid infected/necrotic tissues, irradiated tissues, exposed bone without periosteum, tendon without peritendon, and cartilage without perichondrium.
What are the two main types of skin grafts and their characteristics?
| Type | Full Thickness (FTSG) | Split / Partial Thickness (STSG) |
|---|---|---|
| Basics | Entire Epidermis + Dermis | Entire Epidermis + Partial Dermis |
| Graft | Direct closure or with split thickness grafting | Not needed, will heal spontaneously |
| Healing | Will not heal if not closed | Heals spontaneously |
| Cosmetics | Better | Poor |
| Endurance | Lower chance of graft survival | Higher chance of graft survival |
| Donor sites | Nearby site of similar skin colour and consistency | Thigh, buttocks, forearms |
| Contracture | Primary contracture due to elastin in the dermis after graft is harvested | Secondary contracture due to myofibroblast activity after graft is healed |
| Disadvantages | High risk of graft failure, donor site morbidities | Poor cosmesis |
What are the stages of skin survival after a graft?
The stages of skin survival are:
Plastic imbibition - Passive absorption of nutrients via diffusion.
Inoculation ("To Kiss") ~ Day 3 - Cut ends of vessels on the underside of dermis form connections with the sound bed.
Revascularization ~ Day 5 - New vessels grow into the graft.
What are some reasons for skin graft failure?
Reasons for graft failure can be categorized as follows:
| Type | Reasons |
|---|---|
| Structural | - Haematoma |
| - Seroma | |
| - Shear force | |
| Functional | - Infection |
| - Group A ß-haemolytic Strep leading to Streptokinase and hyaluronidase, which prevents adhesion | |
| Medical error | - Inappropriate bed chosen (e.g., avascular, irradiation region) |
| - Technical error (e.g., upside down graft placement, graft desiccation) |
What are the three types of flaps in flap reconstruction?
What are the characteristics of Relaxed Skin Tension Lines (RSTLs)?
What are the characteristics of Lines of Maximum Extensibility (LME)?
What are the clinical features of flap congestion?
What are the possible causes of flap congestion?
What is the clinical approach to managing flap congestion?
What flap source is used for reconstructing the scalp in sarcoma cases?
Thigh (ALT Flap).
What is the flap source for reconstructing the lower lip affected by squamous cell carcinoma?
Multiple skin components, vastus lateralis muscle, sensory & motor nerves, and vein.
What flap technique is used for tongue reconstruction in tongue cancer?
A 2D flap folded into a 3D flap.
What flap source is used for mandible reconstruction?
Transfer bone to reconstruct the mandible.
What flap source is used for pharynx reconstruction in NPC?
Thigh used (rolled into a tube).
What flap techniques are used for breast reconstruction in breast cancer?
TRAM Flap / DIEP Flap.
What are the two main types of post-mastectomy breast reconstruction?
The two main types are implant-based reconstruction and autologous flap reconstruction.
What is a significant risk associated with texture-surfaced implants?
Texture-surfaced implants are associated with BIA-ALCL (Breast Implant-Associated Anaplastic Large Cell Lymphoma).
What is the main difference between the TRAM flap and the DIEP flap procedures?
The TRAM flap procedure transfers lower abdominal skin, fat, and one of the rectus muscles to reconstruct the breast, while the DIEP flap uses skin and fat from the lower abdomen but spares the rectus muscle, preserving abdominal strength.
What anatomical structures are involved in the TRAM flap procedure?
The TRAM flap procedure involves the superior epigastric pedicle, lower abdominal skin, fat, and one of the rectus muscles.
What are the key components of the DIEP flap procedure?
The DIEP flap procedure involves the skin and fat from the lower abdomen, with the DIEA, DIEV, and perforators dissected from the muscle, while sparing the rectus muscle.
Which flap procedures are indicated on the female torso illustration?
The illustration indicates several flap procedures including DIEP, SIEA, Free TRAM, Pedicled TRAM, T-Dap (Latissimus dorsi muscle), LSGAP/SGAP, and TUG.
What is the procedure for silicone expanders in tissue expansion?
What are the advantages of using silicone expanders?
What are the contraindications for silicone expanders?
What is the purpose of fat injection in breast augmentation?
The purpose of fat injection is for breast augmentation.
What are the steps involved in the harvesting procedure for fat injection?
What is the procedure for re-injecting harvested fat in breast augmentation?
What are the difficulties associated with ear replant in trauma settings?
What management techniques are used in ear replant procedures?
What is microtia?
Microtia is a congenital anomaly of the ear characterized by malformed and small ears.
What is the management approach for microtia?
What are the stages involved in the management of microtia?
What is an alternative method for achieving the best cosmetic result in microtia management?
Cosmetic ears can be attached by glue or osteointegrated buttons for the best cosmetic result.
What defines prominent ears?
Prominent ears are characterized by an ill-defined or loss of the anti-helical fold.
What is the goal of treatment for prominent ears?
The goal of treatment is the reconstruction of the anti-helical fold to bring the ear closer to the head.
What is the definition of a burn?
A burn is a wound caused by externally induced pathological change in energy levels within a tissue, leading to damage.
What are the main sources of energy that cause burns?
The main sources of energy that cause burns include:
Thermal (most common)
Special Burns
What are the immediate priorities of treatment for burns?
The immediate priorities of treatment for burns include:
What are the long-term outcomes to consider in burn treatment?
The long-term outcomes to consider in burn treatment are:
What are the three zones in Jackson's Burn Model?
The three zones in Jackson's Burn Model are:
Zone of Coagulation
Zone of Stasis
Zone of Hyperaemia
What is the significance of the Zone of Stasis in burn management?
The Zone of Stasis is significant in burn management because:
What complications can arise from the Zone of Hyperaemia in burns?
Complications that can arise from the Zone of Hyperaemia in burns include:
What are the mechanical effects of upper airway inhalation injury?
What physiological effects can occur due to upper airway inhalation injury?
What are the potential consequences of upper airway inhalation injury?
What characterizes lower airway inhalation injury?
What systemic effect can result from inhalation injury?
What clinical history clues suggest inhalation injury?
What are the general examination findings for inhalation injury?
What respiratory examination findings indicate inhalation injury?
What is the management priority for patients with inhalation injury?
Secure airway BEFORE fluid resuscitation
What airway management technique is recommended for inhalation injury?
When should fluid resuscitation be initiated in patients with inhalation injury?
What is the primary cause of Carbon Monoxide (CO) poisoning?
CO is a product of incomplete combustion of hydrocarbons, such as indoor burning of charcoal and inefficient indoor heaters.
How does the affinity of Carbon Monoxide (CO) for hemoglobin compare to that of oxygen?
CO has a 240 times greater affinity for hemoglobin compared to oxygen, which significantly reduces the oxygen-carrying capacity of hemoglobin (Hb).
Why is pulse oximeter reading considered misleading in cases of CO poisoning?
Pulse oximeter readings are inaccurate in CO poisoning because they cannot detect CO-Hb, leading to potentially misleading results.
What is the required method to assess CO-Hb levels in suspected CO poisoning cases?
A blood gas reading is required to accurately assess CO-Hb levels, as pulse oximeters are not reliable in this context.
What is the half-life of CO-Hb in room air and how does it change with 100% oxygen?
The half-life of CO-Hb is 3-4 hours in room air, but it can be reduced to 30-90 minutes when given 100% oxygen.
What are the acute management steps for CO poisoning?
The acute management steps include:
What criteria indicate the need for ICU care in CO poisoning cases?
ICU care should be considered if there are features of tissue hypoxia, such as:
What are the indications for considering Hyperbaric Oxygen (HBO) treatment in CO poisoning?
HBO treatment should be considered if there is:
What is the discharge criterion for stable patients after CO poisoning treatment?
Stable patients can be discharged when CO-Hb levels are <10% and they are asymptomatic.
What are the pathophysiological differences between acid burns and alkaline burns?
What factors determine the severity of a burn?
The severity of a burn depends on:
What are the initial management steps for a chemical burn?
What are the clinical features and management of Hydrofluoric Acid burns?
Clinical features:
Management:
What are the major complications associated with electrical burns?
Major complications of electrical burns include:
Close monitoring is essential, including continuous cardiac monitoring and checking urine color for myoglobinuria.
What are the urgent investigations required for a patient with an electrical burn?
Urgent investigations for a patient with an electrical burn include:
What are the main sources of energy that can cause burns?
How does the environment affect the risk of inhalation injuries in burn cases?
What is the relationship between contact time and burn depth?
What is the most effective immediate management for burns?
What is the Rule of Palm used for in burn assessment?
How does the Rule of Nines estimate burn surface area?
What is the Lund Browder chart and its significance in burn assessment?
What is the purpose of the Lund and Browder Chart?
The Lund and Browder Chart is used to estimate the percentage of total body surface area (TBSA) affected by burns, providing a more accurate assessment than simpler methods.
How does the Lund and Browder Chart differ from the Rule of Nines in estimating burn percentage?
The Lund and Browder Chart provides a more detailed assessment by accounting for different body regions and age variations, while the Rule of Nines uses a simpler method with fixed percentages for body sections.
What percentage of total body surface area does the head account for in the Lund and Browder Chart for adults?
In adults, the head accounts for 3.5% of the total body surface area according to the Lund and Browder Chart.
What is the percentage of total body surface area for each arm according to the Rule of Nines?
Each arm accounts for 4.5% of the total body surface area on each side according to the Rule of Nines.
What is the total percentage of body surface area for the anterior trunk in the Rule of Nines?
The anterior trunk accounts for 18% of the total body surface area in the Rule of Nines.
In the Lund and Browder Chart, what percentage does one thigh account for in a 15-year-old?
In a 15-year-old, one thigh accounts for 4.5% of the total body surface area according to the Lund and Browder Chart.
What is the significance of the genitalia area in the Rule of Nines?
The genitalia area accounts for 1% of the total body surface area in the Rule of Nines, which is important for assessing burn severity and treatment needs.
How does the Lund and Browder Chart adjust burn area estimates for different ages?
The Lund and Browder Chart provides specific percentages for burn areas that vary by age, reflecting the differences in body proportions as a person grows.
What are the clinical features of a superficial burn?
How does a superficial dermal partial thickness burn heal?
Heals without surgery in 14 days.
What are the clinical features of a deep dermal partial thickness burn?
What are the characteristics of a full thickness burn?
What is a unique complication of circumferential burns?
Impaired distal limb perfusion and difficult ventilation if over the chest.
What is the cut-off measurement for compartment pressure in circumferential burns?
30 mmHg, measured by Stryker needle.
What are the two treatment options for full thickness burns?
Escharotomy (LA)
Fasciotomy (GA)
What increases fluid requirements in full thickness burns?
Destruction of RBC in skin vessels leads to increased hydrostatic pressure, reduced oncotic sequestration, and increased capillary permeability.
What are the neurovascular features of different burn depths?
| Wound Type | Colour | Blister | Cap. Refill | Sensation | Healing |
|---|---|---|---|---|---|
| Epidermal | Red | No | Brisk | Present | Spontaneous |
| Superficial dermal | Pale pink | Yes | |||
| Deep dermal | Botchy red | Variable | >2 | Reduced | Poor |
| Full thickness | White, waxy leathery | No | Absent | Absent | No |
What are the criteria for transferring paediatric patients to a burn centre?
What burn locations are considered for transfer to a burn centre?
What are the severity criteria for burns that warrant transfer to a burn centre?
What complications may necessitate a burn centre transfer?
What are the immediate treatment principles for burn management?
What is the conservative approach in early management of burns?
What surgical interventions are indicated for early management of burns?
What are the late management considerations for burn patients?
What are the steps involved in the primary survey during acute management of severe burns?
What is the role of fluids in first aid for burn management?
What analgesic is recommended for burn patients in first aid?
What does the secondary survey in burn management involve?
What is the indication for fluid resuscitation in adults and children based on TBSA involved?
What is the formula for calculating fluid resuscitation according to Parkland's Formula?
Fluid resuscitation is calculated as: 2 to 4 mL × Weight (kg) × TBSA%
What is the timing for administering fluid resuscitation for burns greater than 20% TBSA?
What type of fluid is used for resuscitation according to Parkland's Formula?
Hartmann's solution is used for fluid resuscitation.
What is the target urinary output for adults and children during fluid resuscitation?
What are the steps for managing rhabdomyolysis during fluid resuscitation?
Aggressive rehydration (NS & D5)
Urine alkalinization
Osmotic diuresis
What is the immediate treatment for thermal burns?
What is the procedure for creating meshed skin?
The procedure involves expanding the skin by creating holes through a mesher, allowing for an expansion ratio of 1:1.5/1.6.
What are the advantages of using meshed skin?
What are the disadvantages of meshed skin?
What is the structure of the skin substitute Integra?
Integra consists of two layers:
What happens after weeks of placing the collagen layer of the skin substitute?
Blood vessels grow into the collagen layer, creating a neodermis that turns pink. The silicone layer can then be removed for the placement of a skin graft in a second stage operation.
What is Meek Micrografting and when is it preferred?
Meek Micrografting is a grafting technique preferred in total body surface area (TBSA) greater than 30%.
What are the advantages of Meek Micrografting?
What is a disadvantage of Meek Micrografting?
It is time and manpower consuming.
What is a potential consequence of inadequate care in burn scar management?
Formation of bands that can affect activities of daily living (ADL).
What is a management option for burn scars?
Free flap is a management option for burn scars.
What is the Fitzpatrick Scale used for?
The Fitzpatrick Scale is a numerical classification schema for human skin color, categorizing skin types based on their reaction to sun exposure.
What are the six skin types described in the Fitzpatrick Scale?
The six skin types are:
What are the key components of a physical examination for skin lesions?
The key components include:
What does the 'Surface' category in the skin lesion examination refer to?
The 'Surface' category refers to the Size, Shape, and Site of the skin lesion.
What might a darkly pigmented ulcerated lesion indicate?
A darkly pigmented ulcerated lesion may indicate a malignant skin lesion, requiring further evaluation.
What are some special comments to consider during a skin lesion examination?
Special comments to consider include:
What are Seborrheic Keratoses and their histological characteristics?
Seborrheic Keratoses are benign overgrowths of the basal cell layer of the epidermis, characterized histologically by:
What is the clinical presentation of Seborrheic Keratoses?
Seborrheic Keratoses present as benign, pigmented lesions, commonly found in individuals aged 40-50 years and older. They may itch with age and are most commonly located on the head and trunk, particularly in sun-exposed areas. They can appear as single or multiple lesions with a 'stuck-on' appearance, varying in pigmentation from light brown to black, and have a velvety or warty surface.
What are the management options for Seborrheic Keratoses?
Management options for Seborrheic Keratoses include:
What defines Actinic Keratosis and its pathophysiology?
Actinic Keratosis is a pre-malignant lesion characterized by atypia of the epidermis that does not involve full thickness. It results from UV radiation damage to keratinocytes due to repeated sun exposure, particularly UV-B, leading to thickening and scaling of the keratin layer, resulting in hard scaly plaques.
What is the clinical significance of Actinic Keratosis?
Actinic Keratosis is a pre-malignant lesion with a 25% risk of transforming into squamous cell carcinoma (SCC) if untreated. It is more common in older individuals with chronic sun exposure and light skin.
What are the physical examination findings for Actinic Keratosis?
Physical examination findings for Actinic Keratosis include:
What are the management options for Actinic Keratosis?
Management options for Actinic Keratosis include:
What is Bowen's Disease and its clinical significance?
Bowen's Disease is a pre-malignant lesion, also known as SCC in-situ, primarily affecting females. It is associated with HPV types 16 and 18 and has a risk of evolving into squamous cell carcinoma (SCC) in 10-20% of cutaneous lesions and over 20% of mucosal lesions. It is characterized by an erythematous plaque-like lesion with sharply demarcated red and scaly borders, typically measuring 1-3 cm in diameter, found on skin and mucous membranes.
What are the key features of Keratoacanthoma?
Keratoacanthoma is a pseudo-benign or pseudo-malignant lesion characterized by a benign overgrowth of hair follicle cells that produces a central keratin plug. It is an epithelial neoplasm with atypical keratinocytes in the epidermis, often associated with HPV, UV radiation, and chemical carcinogens. It typically presents as a rapidly growing lesion that forms within 6 weeks and may regress if left untreated, leaving a depressed scar.
What are the clinical presentations and differential diagnoses for Keratoacanthoma?
Keratoacanthoma presents as a rapidly growing lesion, often found in males over 50 years old. Important differential diagnoses include:
What are the physical examination findings for Keratoacanthoma?
Physical examination findings for Keratoacanthoma include:
| Feature | Description |
|---|---|
| Appearance | - Sun-exposed areas, well-circumscribed, dome-shaped with a central keratin crater resembling a volcano. Normal skin color except for the central core (brown/black due to keratin). |
| Palpation | - Firm consistency except for the central core containing a very hard keratin plug; fully mobile over deep tissues. |
| Completion | - Look for similar lesions elsewhere and assess impact on activities of daily living (ADL). |
What are the management options for Keratoacanthoma?
Management options for Keratoacanthoma include:
What are the risk factors for malignant transformation in naevi?
What are the characteristics of acquired naevi?
What defines functional naevi?
What are the features of compound naevi?
What characterizes intradermal naevi?
What are the features of congenital melanocytic naevi?
What is the risk of transformation for congenital melanocytic naevi?
What is the definition of congenital melanocytic naevi?
What is the pathophysiology of congenital naevi?
What is a lipoma and where can it occur?
A lipoma is a benign tumor arising from adipose tissue and can occur anywhere there is fat in the body.
What is the differential diagnosis for lipomas, especially when they are larger than 5 cm?
The differential diagnosis for lipomas, particularly when they are larger than 5 cm, is liposarcoma.
What syndrome is associated with multiple painful lipomas?
Dercum's Disease is associated with multiple painful lipomas.
What are the clinical features of a lipoma?
The clinical features of a lipoma include:
What imaging techniques are used for investigating lipomas?
Imaging techniques used for investigating lipomas include Ultrasound (USG) and MRI.
What is the management approach for lipomas?
The management of lipomas includes:
What are sebaceous cysts also known as?
Sebaceous cysts are also known as epidermal cysts.
What is the definition of a sebaceous cyst?
A sebaceous cyst is an inclusion cyst due to the implantation of epidermis into the dermis, originating from the proliferation of epidermal cells from the infundibulum of hair follicles.
What are the histological features of sebaceous cysts?
The histological features of sebaceous cysts include:
What are the clinical features of sebaceous cysts?
The clinical features of sebaceous cysts include:
What complications can arise from sebaceous cysts?
Complications from sebaceous cysts can include trauma and infection.
What syndrome is associated with sebaceous cysts?
Gardner Syndrome (Familial Adenomatous Polyposis - FAP) is associated with sebaceous cysts.
What is the management for sebaceous cysts?
The management of sebaceous cysts includes:
What are skin tags and where are they commonly located?
Skin tags are small flesh-colored growths that hang off the skin, often with stalks. They are most commonly found on the neck, armpits, and groins, particularly in older individuals and in areas where skin rubs against skin or clothing.
What are the clinical features of skin tags?
Skin tags are most common in older people and typically occur in areas where skin rubs against skin or clothing.
What is the origin and nature of warts?
Warts are viral in origin, caused by the Human Papillomavirus (HPV), and are contagious.
What are the characteristic features of warts?
Warts often have a 'cauliflower' appearance, characterized by a rough, raised growth.
What are the common treatment options for warts?
Treatment options for warts include:
What is the most common age range for the occurrence of Basal Cell Carcinoma (BCC)?
Basal Cell Carcinoma (BCC) most commonly occurs between 40-90 years old.
What is the most common type of skin cancer?
Basal Cell Carcinoma (BCC) is the most common skin cancer regardless of ethnicity.
Where do a large proportion of BCC cases occur in Hong Kong?
A large proportion of BCC cases in Hong Kong occur in non-sun exposed areas.
What is the primary site for Basal Cell Carcinoma?
The primary site for Basal Cell Carcinoma (BCC) is the head and neck, accounting for 85% of cases.
What are the characteristics of Basal Cell Carcinoma in terms of metastasis?
Basal Cell Carcinoma is locally destructive but rarely metastasizes.
What are some pre-malignant lesions associated with Basal Cell Carcinoma?
Pre-malignant lesions associated with BCC include Actinic Keratosis and Bowen's Disease (SCC in-situ).
What is the histological appearance of Basal Cell Carcinoma?
Histologically, BCC is characterized by sheets/nests of small round basophilic cells and peripheral palisading.
What are the congenital predisposing factors for Basal Cell Carcinoma?
Congenital predisposing factors for BCC include Xeroderma pigmentosum and Gorlin Syndrome.
What is the inheritance pattern of Gorlin Syndrome?
Gorlin Syndrome is inherited in an autosomal dominant pattern.
What are the main features of Gorlin Syndrome?
The main features of Gorlin Syndrome include multiple BCC, palmar pits, odontogenic cysts, bifid ribs, calcification of falx cerebri, and learning difficulties.
What is the most common clinical subtype of Basal Cell Carcinoma?
The most common clinical subtype of BCC is Nodular/Nodulo-ulcerative, which is characterized by a well-defined rolled, pearly edge and central ulceration (Rodent ulcer).
What distinguishes pigmented Basal Cell Carcinoma from malignant melanoma?
Pigmented Basal Cell Carcinoma contains melanin and can be confused with malignant melanoma, but it is typically found in Hong Kong.
What are the characteristics of sclerosing Basal Cell Carcinoma?
Sclerosing Basal Cell Carcinoma is flat/depressed with an ill-defined edge and may be ulcerated, occurring later in the disease progression.
What are the features of superficial Basal Cell Carcinoma?
Superficial Basal Cell Carcinoma presents as erythematous scaly patches and can be confused with Bowen's Disease.
What are the common sites for basal cell carcinoma (BCC) inspection?
What are the typical appearances of basal cell carcinoma (BCC) in Caucasian patients?
What does palpation reveal in cases of basal cell carcinoma (BCC)?
What is the management recommendation for basal cell carcinoma (BCC) lesions less than 2cm?
What is the recommended excision margin for basal cell carcinoma (BCC) lesions greater than 2cm or morpheaform lesions?
What is Mohs micrographic surgery and how is it performed?
What are the non-surgical management options for basal cell carcinoma (BCC)?
What is the typical treatment cycle for radiotherapy in basal cell carcinoma (BCC)?
What is the incidence of Squamous Cell Carcinoma (SCC) compared to Basal Cell Carcinoma (BCC)?
SCC has a 1/3 incidence compared to BCC.
From which cells does Squamous Cell Carcinoma arise?
SCC arises from epidermal cells that normally migrate to the skin surface to form the superficial keratinizing squamous layer.
What are the degrees of differentiation in Squamous Cell Carcinoma?
The degrees of differentiation in SCC are:
What are some congenital and acquired predisposing factors for Squamous Cell Carcinoma?
Congenital factors:
Acquired factors:
What is the cancer risk associated with Xeroderma Pigmentosum?
Individuals with Xeroderma Pigmentosum have a 100% risk of developing Squamous Cell Carcinoma, as well as risks for Basal Cell Carcinoma and Malignant Melanoma.
What are the poor prognostic indicators for Squamous Cell Carcinoma?
Poor prognostic indicators for SCC include:
What is the typical lifespan of children with Xeroderma Pigmentosum?
Children with Xeroderma Pigmentosum typically have a limited lifespan and may die before the age of 20 due to the disease.
What is the recurrence rate of Squamous Cell Carcinoma based on differentiation?
The recurrence rate of SCC is:
What are the early and late disease appearances of skin lesions in physical examination?
Early disease: Red scaly patches
Late disease: Nodular lesions with vascular (red-brown) appearance, raised and everted edges, possible erosion of facial architecture, and central ulceration.
What are the standard surgical practices for excising skin lesions based on risk levels?
What factors increase the risk for lymph node metastasis in skin lesions?
The risk for lymph node metastasis is small (<1%) but increases with:
What are the indications for using radiotherapy in the management of skin lesions?
Radiotherapy is indicated for:
What is Mohs's Micrographic Surgery and when is it used?
Mohs's Micrographic Surgery is used for skin lesions located in special areas such as eyelids, ears, or nasolabial folds, particularly when there is a risk of lymph node metastasis or when the lesion is recurrent.
What is the epidemiology of malignant melanoma?
What are the pathological features of malignant melanoma?
What are the congenital predisposing factors for malignant melanoma?
What are the acquired predisposing factors for malignant melanoma?
What are the prevention strategies for malignant melanoma?
What are the characteristics of Superficial Spreading melanoma?
What is the most common site for Superficial Spreading melanoma in women?
The most common site for Superficial Spreading melanoma in women is the leg.
What is the prevalence of Acral Lentiginous melanoma in Asians?
Acral Lentiginous melanoma is most common in Asians, accounting for 5-10% of cases, and represents 50% of all melanoma cases in Asians.
What are the sites commonly affected by Acral Lentiginous melanoma?
Common sites for Acral Lentiginous melanoma include the subungual area, palm, and sole.
What is the Glasgow 7-Point Checklist used for?
The Glasgow 7-Point Checklist is recommended for primary care professionals to evaluate pigmented skin lesions for possible melanoma.
What does a score of ≥3 on the Glasgow 7-Point Checklist indicate?
A score of ≥3 on the Glasgow 7-Point Checklist is suggestive of possible melanoma, warranting urgent referral.
What are the major features in the Glasgow 7-Point Checklist?
The major features (2 points each) are:
What are the minor features in the Glasgow 7-Point Checklist?
The minor features (1 point each) are:
What are the characteristics of Nodular melanoma?
Nodular melanoma is characterized by being protruding with well circumscribed margins.
What is Lentigo Maligna and its development process?
Lentigo Maligna is a type of melanoma that is pre-existing and can develop into intra-lesional ulcer or colour changes.
What are the suspicious features of malignant melanoma according to the ABCDE criteria?
What are the characteristics of Nodular Melanoma?
What are some late features of malignant melanoma?
What is the significance of Breslow's thickness in melanoma prognosis?
Breslow's thickness is a key prognostic indicator for melanoma, with worse prognosis associated with thicker lesions. For example:
| Breslow's thickness | 10-year survival (%) |
|---|---|
| <0.76 mm | 92 |
| <3 mm | 50 |
| <4 mm | 30 |
| Lymph node involvement | <40 (8-year survival) |
What are the principles of excision for melanoma?
What systemic modalities are used in the workup of melanoma?
Why is Clark's level of invasion not as useful as Breslow's thickness for prognosis?
Clark's levels of invasion are less useful because:
What is the procedure for surgical wide local excision for primary lesions?
The procedure involves:
What are the safety margins for tumor thickness according to UK BAD and NCCN guidelines?
| Tumor thickness | Safety margins (UK BAD) | Safety margins (NCCN) |
|---|---|---|
| In-situ | 0.5cm | 0.5-1cm |
| <1mm T1 | 1cm | 1cm |
| 1-2mm T2 | 1-2cm | 1-2cm |
| 2-4mm T3 | 2-3cm | 2cm |
| >4mm T4 | 3cm | 2cm |
What is the procedure for Sentinel Lymph Node Biopsy (SLNB)?
The procedure for Sentinel Lymph Node Biopsy involves:
Note: The frozen section for melanoma is not reliable and is not used.
What targeted therapy is used for BRAF V600E mutation in melanoma?
Targeted therapy for BRAF V600E mutation includes:
What are the characteristics and treatment of Extramammary Paget's Disease (EMPD)?
Extramammary Paget's Disease (EMPD) is characterized by:
Treatment involves:
What are the two types of vascular anomalies based on their appearance at birth?
What is the pathophysiology of vascular malformations?
How do vascular malformations typically behave in terms of growth?
Vascular malformations tend to remain static but grow in proportion with the patient.
What is Klippel-Trenaunay Syndrome associated with?
Klippel-Trenaunay Syndrome is associated with tissue and bone hypertrophy.
What are the clinical presentations of Port Wine Stain (Capillary Naevi)?
What are some clinical features of Sturge-Weber Syndrome related to the CNS?
What are the ocular features associated with Sturge-Weber Syndrome?
What endocrine issue is associated with Sturge-Weber Syndrome?
Growth hormone (GH) deficiency is associated with Sturge-Weber Syndrome.
What is the treatment for vascular malformations like Port Wine Stain?
The treatment involves Pulse Dye Laser (PDL) therapy, which works by:
What are the expected outcomes of Pulse Dye Laser treatment for vascular malformations?
What is a haemangioma?
A haemangioma is a benign vascular neoplasm of unknown cause, often appearing as a raised, erythematous lesion with an irregular border.
What are the characteristics of capillary haemangioma?
Capillary haemangioma is associated with AW/PHACE syndrome and typically presents as a raised, erythematous but non-blanchable lesion with an irregular border.
What is the natural disease history of haemangiomas?
Haemangiomas commonly appear in the first few weeks after birth, with 30% presenting at birth. They grow rapidly, often faster than the child, and typically undergo involution, with 50% resolving by 5 years and 90% by 9 years.
What complications can arise from haemangiomas?
Complications of haemangiomas include:
What is the Kasabach-Merritt Phenomenon?
The Kasabach-Merritt Phenomenon is characterized by a triad of giant haemangioma, thrombocytopenia, and consumptive coagulopathy, resulting from platelet trapping in the vascular tumor, leading to thrombocytopenia.
What investigations are used for haemangiomas?
Investigations for haemangiomas include:
| Investigation |
|---|
| CBC x PLT |
| Clotting |
| GI: USG abdomen & liver |
| CT Abdomen |
| CNS: Cranial USG |
| MRI Brain |
| Resp: Laryngoscopy |
| CV: Echocardiogram |
What are the treatment options for asymptomatic haemangiomas?
Treatment options for asymptomatic haemangiomas include:
| Indication | Treatment Options |
|---|---|
| Haemangioma at critical sites | Reassurance |
| PHACES syndrome | No treatment needed |
| Very large size / Rapidly growing | Pharmacological: β-Blocker (PO/Topical Propranolol), Topical timolol |
| Permanent disfigurement | Procedural: Pulse dye laser (if ulcerated), Surgery |
| Kasabach-Merritt Phenomenon | Systemic Steroids, Interferon alpha |
What are the types of wound healing?
| Type of Healing | Description |
|---|---|
| Primary intention | - Wound closure by direct approximation, pedicle flap, or skin graft. |
| Secondary intention | - Wound left open to heal spontaneously, relying on contraction & epithelization. |
| Tertiary intention | - Delayed wound closure after a period of time. |
What are the stages of wound healing and their timeframes?
| Stage | Timeframe | Description |
|---|---|---|
| Haemostasis & Coagulation | First few hours | - Blood clots form. |
| Inflammatory phase | D1-D4 | - Symptoms: Redness, Heat, Swelling, Pain, Loss of function. |
| - D1: Neutrophil Infiltration. | ||
| - D2-3: Monocytes → Macrophages release tissue growth factors. | ||
| Proliferative phase | D4-D42 (6 weeks) | - Rapid gain of tensile strength in the wound. |
| - D4: Fibroblast infiltration. | ||
| - ↑ Rate of collagen synthesis for 42-60 days. | ||
| - Proliferate & replace provisional matrix by collagen-rich granulation tissue. | ||
| Remodelling phase | 3 weeks onwards | - Maturation by intermolecular cross-linking of collagen → flattening of scar. |
| - Dynamic and ongoing process. |
What are the different types of wound dressings?
Antibacterial medication
Medication | Impact on Wound Healing |
|---|---|
Bacitracin® and Neosporin® | - Moist environment conducive to epithelization. |
Silver sulfadiazine (Slivadene®) and Mafenide Acetate (Sulfamylon®) | - For burns/wounds with eschar. Can alter the time required for each stage. |
- Antibacterial activity penetrates eschar. |
Splinting and casting
Immobilization promotes healing.
Negative pressure wound therapy
Reduces exudate and encourages wound healing
List the methods of wound closure in order of increasing complexity according to the Reconstructive Ladder.
Healing by Secondary Intention
Direct Closure (primary intention) + delayed direct closure
Skin Graft
Local or Regional Flap
Distant Pedicled Rotate Flap
Free Flap (with microsurgery)
What are the pros of using autologous flap reconstruction?
The pros of autologous flap reconstruction include:
What are the cons of using autologous flap reconstruction?
The cons of autologous flap reconstruction include:
Describe the pedicled flap TRAM procedure.
In the pedicled flap TRAM procedure:
What is the DIEP flap and why is it considered the current gold standard?
The DIEP flap (Deep Inferior Epigastric Perforator Flap) is considered the current gold standard because:
What are some other options for autologous flap reconstruction?
Other options for autologous flap reconstruction include:
What are the pros and cons of implant-based breast reconstruction?
Pros of implant-based reconstruction:
Cons of implant-based reconstruction:
What dressing is recommended for thermal burns?
What is the typical healing time for most wounds?
Most wounds heal by themselves in 7-15 days.
What is the primary care instruction for burns?
Keep the burn clean to promote healing.
What are the characteristics of biological dressings for partial thickness burns?
Biological dressings require no change of dressing, are only for partial thickness burns expected to heal spontaneously, and are made from processed amniotic membrane which accelerates burn healing.
What safety measures are taken for biological dressings?
Patients and donors are screened for viral diseases and other risk factors before using biological dressings.
How is a biological dressing applied?
The biological dressing adheres to the wound when applied and is performed only once to twice, flaking off when the burn has healed.
What materials are used in surgery for full thickness burns?
Surgery for full thickness burns uses autografts or alternatives.
What is the method of tangential excision in wound debridement?
Tangential excision involves removing eschar and excising up to the bleeding tissue (viable dermal layer).
What is the procedure for taking a skin graft?
The procedure involves using a skin graft knife to take a thin layer of skin at the mid dermis level, leaving behind bleeding skin that will heal by itself.
What is the purpose of wound debridement in the context of burn treatment?
Wound debridement, including tangential and fascial excision, is performed to remove non-viable tissue and promote healing of the wound.
What local factors affect wound healing?
What systemic factors affect wound healing?
What is the function of wound dressings?
What are the two main types of scars discussed in plastic surgery?
Hypertrophic scars and Keloid scars are the two main types.
What are management options for scars?
Non-surgical management options
massage and moisture
compression pressure garments
silicone sheets or gels
intralesional corticosteroid injections
laser
cryotherapy
Surgical management options
scar excision + adjuvant therapies (radiation therapy and pressure therapy)
What is a major distinction between hypertrophic scars and keloid scars?
What is the primary function of the lymphatic system?
The primary functions of the lymphatic system include:
What is lymphoedema?
Lymphoedema is defined as the accumulation of proteinaceous fluid within the interstitial compartment, which occurs secondary to abnormalities in the lymphatic transport system.
What is Stewart-Treves Syndrome?
Stewart-Treves Syndrome is associated with lymphangiosarcoma that can occur more than 10 years after the onset of lymphoedema and is characterized by a poor prognosis.
What are the secondary causes of lymphoedema?
Secondary causes of lymphoedema include:
Infection: Such as filariasis caused by Wucheria Bancrofti, rare in developed countries.
Post-cancer: Resulting from post-lymph node dissection
Radiotherapy
??? Inflammation: Associated with chronic venous ulcers or DVT/trauma.
What are the stages of Lymphoedema according to the International Society of Lymphology (ISL)?
The stages of Lymphoedema are as follows:
| Stage | Presentation | Increase in limb volume |
|---|---|---|
| Stage 0 Latent Subclinical Stage | No overt swelling, but lymphatic pathways have been disrupted | - |
| Stage 1 Early Stage | Mild pitting oedema that resolves with elevation | <20% increase |
| Stage 2 | Swelling that does not resolve with elevation; less evidence of pitting as fibrosis develops | 20-40% increase |
| Stage 3 (Late Stage) | Non-pitting with skin changes such as papillomata, fibrosis, and hyperkeratosis | >40% increase |
What are the methods used for simple assessment of lymphoedema?
What are common clinical features of lymphoedema?
Common clinical features of lymphoedema include:
Pitting or non-pitting oedema
Skin ulceration
Pain
What are the primary causes of lymphoedema?
** defined by age of onset
Lymphoedema Congenita: Onset within 2 years of birth due to VEGFR3 gene mutation, often showing severe hypoplasia or aplasia.
Lymphoedema Praecox (Meige's Disease): Onset between 2-35 years, most common type of primary lymphoedema, typically unilateral, and may show hypoplasia on lymphangiography.
Lymphoedema Tarda: Onset after 35 years, typically shows hyperplasia on lymphangiography.
What are the radiological investigations for diagnosing lymphoedema?
Lymphoscintigraphy (gold standard): A radioactive tracer is injected intradermally or subfascially. Delayed or absent radiotracer suggests lymphatic abnormality.
MRI lymphangiogram: visualize diffuse and subcutaneous oedema and may replace lymphoscintigraphy in the future, though it is limited by availability.
ICG lymphography: A dye is injected intradermally and taken up by lymphatic capillaries, allowing for real-time imaging of superficial lymphatic flow, which is staged based on lymphatic flow patterns.
** direct/ indirect lymphangiography is NO LONGER USED: involves direct cannulation or lymphatic vessels with injection of oil/ water soluble contrast —> potentially further damaging the lymphatics
What are the management options for lymphoedema?
Conservative management: complete decongestive therapy
Component | Description |
|---|---|
Manual Lymphatic Drainage | Specialized massage to redirect lymph flow |
Compression | - Multilayer inelastic lymphoedema bandaging / compression garment |
Skin Care | - Antiseptic wash |
- Emollients | |
Remedial Exercises | - Elevation and muscle action |
Surgical management
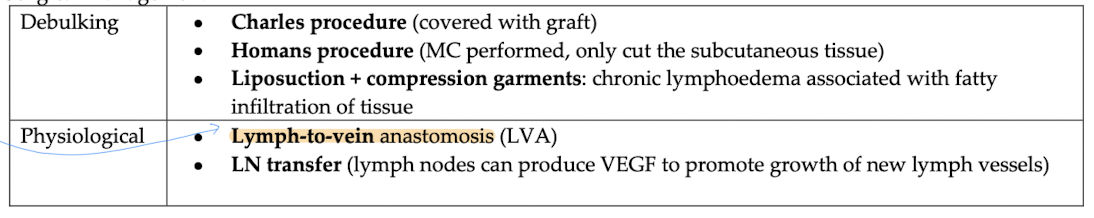
** details see notes!!!