Click to see answer
📌 Pathogens are present in very low concentrations (e.g., <1 per 10,000–100,000 L).
📌 Pathogen testing is complex, costly, and impractical for routine monitoring.
📌 It's more effective to frequently use a simple test for a harmless indicator than to rarely run complicated pathogen tests.
Click to see question
📌 Pathogens are present in very low concentrations (e.g., <1 per 10,000–100,000 L).
📌 Pathogen testing is complex, costly, and impractical for routine monitoring.
📌 It's more effective to frequently use a simple test for a harmless indicator than to rarely run complicated pathogen tests.
📌 It is NOT a faecal indicator.
📌 It measures general microbiological quality and biofilm formation.
📌 It is used as a process control indicator to monitor treatment effectiveness and distribution system cleanliness.
📌 The initial lower temperature allows for resuscitation of stressed or injured bacteria before selective incubation at 44°C for faecal coliforms.
⭐16. Explain the roles of the following indicators in one sentence each:
E. coli: Recent faecal contamination.
Enterococci: Remote faecal contamination (survives longer).
HPC: General cleanliness and process control.
Total coliforms: Treatment failure or post-treatment contamination.
C. perfringens: Historical faecal contamination.
📌18. What is the solution to the problem of pathogen detection?
The solution is to use indicator organisms (like E. coli) to estimate the removal of pathogens through water treatment processes and to indicate faecal contamination.
📌22. Why can one single indicator organism not fulfil all roles?
Because different indicators have different strengths. For example, some indicate recent contamination, while others indicate historical contamination or treatment efficacy. A range of organisms is needed for different purposes.
⭐26. How are faecal coliforms defined?
They are coliforms that can ferment lactose at the higher temperature of 44°C within 48 hours. They can also grow in the presence of bile salts or similar surface agents that inhibit non-intestinal bacteria.
📌 Faecal indicators: E. coli, Enterococci, Clostridia.
📌 Process indicators: Pseudomonas aeruginosa, HPC.
📌 Ingestion (Drinking): e.g., Vibrio cholerae, Salmonella, Norovirus.
📌 Inhalation/Aspiration (Aerosols): e.g., Legionella pneumophila.
📌 Contact (Bathing/Skin): e.g., Pseudomonas aeruginosa, Schistosoma.
📌 Its spores are highly resistant to disinfection and environment.
📌 It indicates historical or remote faecal contamination.
📌 It is useful for validating removal of resistant pathogens (e.g., viruses, protozoa).
📌 Recent faecal contamination → immediate risk to public health.
⭐24. What is the general biochemical definition of a coliform?
A Gram-negative, rod-shaped, non-spore-forming bacterium that ferments lactose with acid and gas production within 48 hours at 35-37°C and is oxidase-negative.
📌25. Why is the oxidase test important in confirming coliforms?
To rule out bacteria like Aeromonas spp., which can ferment lactose at 35°C but are oxidase-positive, unlike true coliforms.
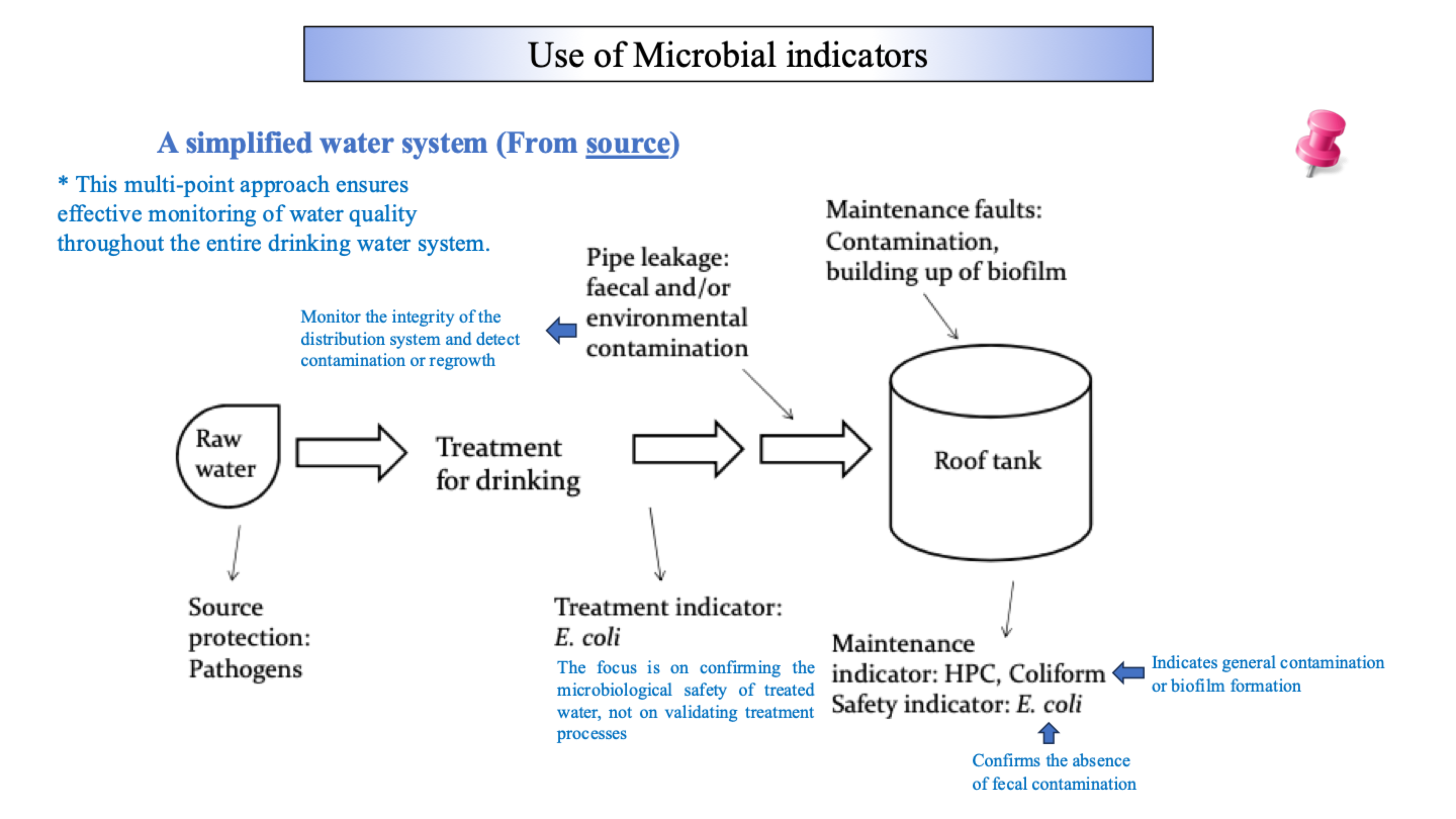
📌31. use of microbial indicators at a simplified water system (from source)
📌 It is exclusively of faecal origin (gut of warm-blooded animals).
📌 It is always present in high numbers in faeces.
📌 It does not multiply in natural waters.
📌 It is easy to detect with simple tests (e.g., MUG test → fluorescence under UV).
📌 Thermotolerant coliforms include E. coli and other bacteria like Klebsiella, which can come from non-faecal sources (e.g., plants, paper mills).
📌 E. coli is a subset of thermotolerant coliforms and is a specific marker of faecal pollution.
📌 They must ferment lactose with acid and gas production within 48 hours at 35–37°C.
📌 E. coli produces the enzyme β-glucuronidase, which hydrolyzes MUG to produce fluorescence under UV light.
📌 They inhibit Gram-positive bacteria and other background flora, selecting for Gram-negative coliforms.
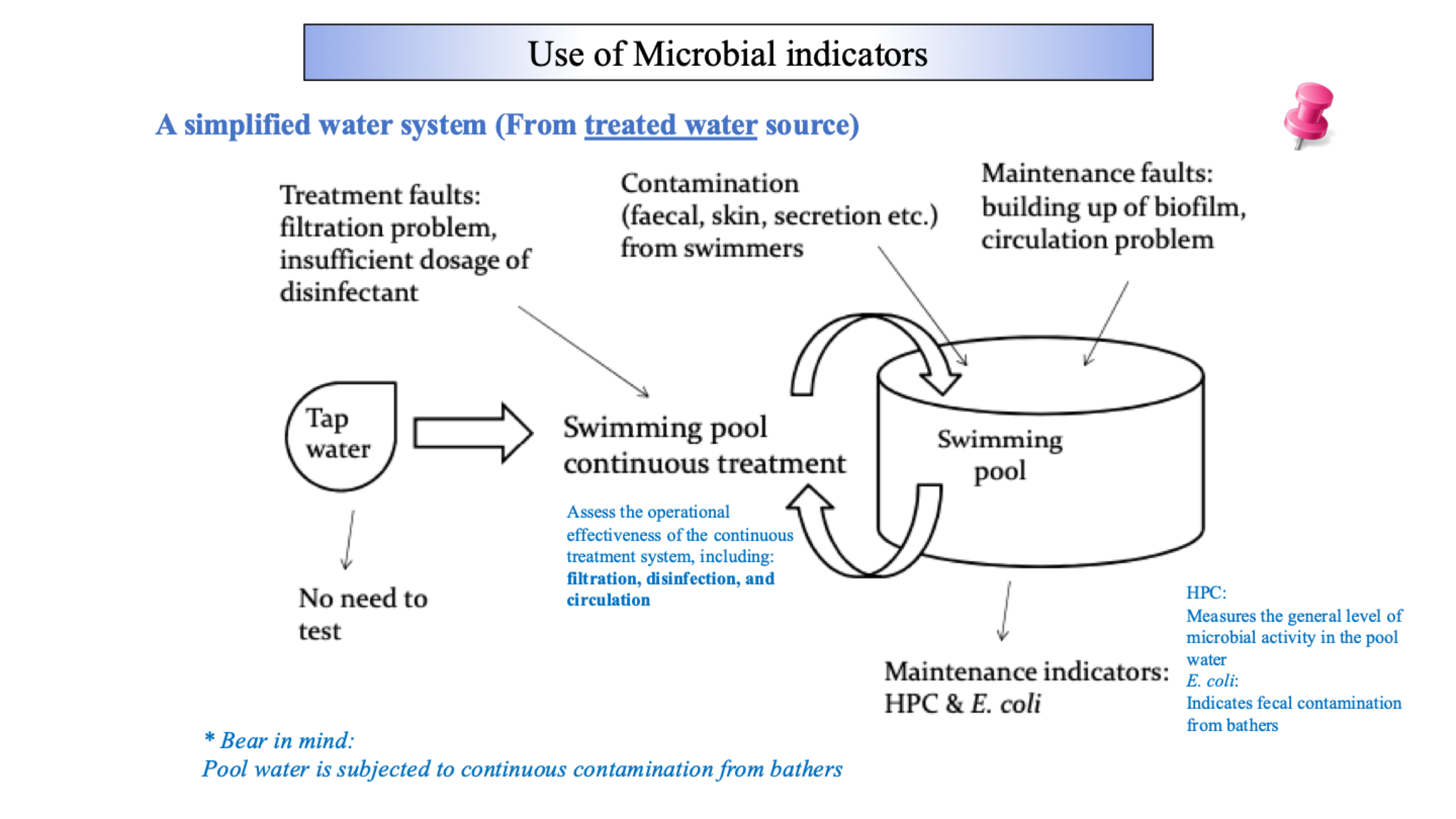
📌 Continuous contamination from bathers, inadequate disinfection, or biofilm buildup.
⭐13. What is the difference between a 2-class and 3-class sampling plan?
📌 2-class plan: Uses a single limit m. Samples are either acceptable (≤m) or defective (>m). Used for zero-tolerance organisms (e.g., E. coli).
📌 3-class plan: Uses two limits: m (acceptable) and M (unacceptable). Allows for a margin of defective samples. Used for quantitative counts (e.g., HPC).
📌 Proposed in the late 19th century after Escherich discovered Bacterium coli (now E. coli) in infant faeces.
📌 Schardinger (1892) first suggested its use as evidence of faecal pollution.
⭐17. Why is direct pathogen detection in water not routinely performed?
insufficient data to set performance target for all potentially waterborne pathogens that water quality targets are not developed for pathogens
Monitoring finished water for pathogens is not considered a feasible or cost effective option because pathogen concentration equivalent to tolerable level of risk are typically less than 1 organism per 10^4 - 10^5 (usually in low concentrations)
pathogen measurement, when performed, is generally best carried out at location where pathogens are at highest concentration (generally raw water)
⭐21. List the seven ideal criteria for a faecal indicator organism.
Not be pathogenic itself.
Be universally present in faeces in large numbers.
Not multiply in natural waters.
Persist in water similarly to faecal pathogens.
Be present in higher numbers than pathogens.
Respond to water treatment similarly to pathogens.
Be easily detected by simple, cheap culture methods.
⭐29. For bottled natural mineral water, what are the two categories of indicators used?
A. Faecal Indicators: E. coli, Total coliforms, Enterococci, Spore-forming sulphite-reducing anaerobes.
B. Process Control Indicators: Pseudomonas aeruginosa, Aerobic mesophilic count (HPC), Total coliforms.
⭐30. Explain the rationale for choosing each of these indicators (faecal + process control):
a. E. coli: The best indicator of recent faecal contamination. It does not survive long in the environment.
b. Total Coliforms: Indicate general contamination. Their presence suggests contamination either at the source or during the packaging process, as they should not be present in a protected mineral water source.
c. Enterococci: A subgroup of faecal streptococci that survive longer in the environment than E. coli. They indicate remote (older) faecal contamination.
d. Spore-forming sulphite-reducing anaerobes (e.g., Clostridium): Their spores are highly resistant to environmental stress and disinfection. They indicate historical faecal contamination that could have happened a long time ago.
e. Pseudomonas aeruginosa: Not part of natural mineral water flora. Its presence indicates contamination from the environment or during packaging.
f. Aerobic Mesophilic Count / HPC: Part of the natural flora. Used as a process management indicator. A rising count indicates problems with cleanliness, stagnation, or biofilm development in the system.
Indicator | What it Indicates | Key Trait |
|---|---|---|
E. coli | Recent faecal contamination | MUG+, Urease- |
Enterococci | Remote faecal contamination | Survives longer than E. coli |
Clostridium | Historical faecal contamination | Forms resistant spores |
HPC | General cleanliness & biofilms | Not faecal-specific |
Total Coliforms | General contamination (source/packaging) | Lactose fermentation at 35°C |
📌32. use of microbial indicators at a simplified water system (from treated water source)
📌19. What is the core "Indicator Concept"?
It involves using non-pathogenic, easily detectable microorganisms to indicate that faecal contamination has occurred, which implies a potential public health risk. The concept is based on the fact that most waterborne pathogens are faecally derived.
⭐20. What are the four specific roles of indicator organisms? Answer:
Source Assessment: Determining the quality of the raw water source.
Validation of Treatment Process: Verifying that the water treatment is effective.
Operational & Routine Monitoring: Continuously checking the system (e.g., in pipelines or swimming pools).
Verification of the End Product: Ensuring the final water is safe (e.g., from a tap).
⭐23. In a simplified water system, what does a high HPC (Heterotrophic Plate Count) indicate?
It indicates general biological activity, which can signal:
Biofilm buildup in the distribution system.
General contamination (not necessarily faecal).
Ineffective disinfection or treatment processes.
It is a maintenance indicator, not a faecal indicator.
📌27. Why are synthetic surfactants (e.g., in Membrane Lauryl Sulphate Broth) used instead of bile salts?
Because bile salts are a biological source and their composition can vary, making them unreliable. Synthetic surfactants provide a more consistent and effective way to inhibit background flora (especially Gram-positive bacteria).
⭐28. What are the key characteristics used to identify E. coli?
It is a species of faecal coliform.
MUG-positive: Produces the enzyme β-glucuronidase (glows under UV light).
Urease-negative: Does not produce urease (differentiates it from Klebsiella).
Indole-positive: Produces indole from tryptophan.
Ferments lactose at 44°C.